Clinical significance of routine lacrimal sac biopsy during dacryocystorhinostomy: A comprehensive review of literature
DOI:
https://doi.org/10.17305/bjbms.2016.1424Keywords:
lacrimal sac, histopathology, specific pathology, chronic dacryocystitis, dacryocystorhinostomyAbstract
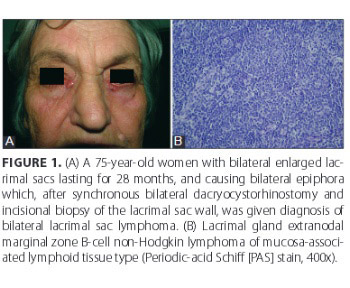
The main purpose of this paper is to provide the information about the incidence and types of pathology of secondary acquired obstructions of the lacrimal excretory outflow system caused by primary lacrimal sac non-neoplastic and neoplastic lesions. After a thorough literature search, 17 case-control studies were found and selected, data were extracted and categorized, to evaluate specific lacrimal sac pathology mimicking inflammation. A total of 3865 histopathologically examined lacrimal sac wall biopsy specimens from 3662 patients, taken during dacryocystorhinostomy for clinically presumed primary chronic dacryocystitis, were analyzed. The most common reported histopathological finding was non-specific chronic inflammation with or without fibrosis (94.15% of cases). Lacrimal sac-specific pathologies were present in 226 (5.85%) cases. Unsuspected lacrimal sac-specific pathologies were present in 55/226 (24.34%) cases. Almost 45% of primary lacrimal sac malignant neoplasms were not suspected, preoperatively and intraoperatively. Tumor-like lesions of the lacrimal sac were the most common pathology found: (1) lacrimal stones-dacryoliths, (2) pyogenic granuloma, (3) granulation tissues, (4) reactive lymphoid hyperplasia, and (5) lacrimal sac-specific inflammation (Wegener’s granulomatosis and sarcoidosis). Neoplastic pathology was found in 55/3865 (1.42%) lacrimal sac wall biopsy specimens; of those, malignant cases were 2.24 times more frequent than benign. Lymphoma was the most common preoperatively unsuspected or intraoperatively unexpected neoplastic pathology. This analysis of the relevant literature highlights the value of routine lacrimal sac biopsy during surgery for clinically presumed primary acquired nasolacrimal duct obstruction.
Citations
Downloads
References
Bartley GB. Acqiured lacrimal drainage obstruction: An etiologic classification system, case reports, and a review of the literature. Part 3. Ophthal Plast Reconstr Surg 1993;9(1):11-26. http://dx.doi.org/10.1097/00002341-199303000-00002.
Mandeville JT, Woog JJ. Obstruction of the lacrimal drainage system. Curr Opin Ophthalmol 2002;13(5):303-9. http://dx.doi.org/10.1097/00055735-200210000-00003.
Linberg JV, McCormick SA. Primary acquired nasolacrimal duct obstruction. A clinicopathologic report and biopsy technique. Ophthalmology 1986;93(8):1055-63. http://dx.doi.org/10.1016/S0161-6420(86)33620-0.
Mauriello JA Jr, Palydowycz S, DeLuca J. Clinicopathologic study of lacrimal sac and nasal mucosa in 44 patients with complete acquired nasolacrimal duct obstruction. Ophthal Plast Reconstr Surg 1992;8(1):13-21. http://dx.doi.org/10.1097/00002341-199203000-00002.
Tucker N, Chow D, Stockl F, Codure F, Burnier M. Clinically suspected primary acquired nasolacrimal duct obstruction: Clinicopathologic review of 150 patients. Ophthalmology 1997;104(11):1882-6. http://dx.doi.org/10.1016/S0161-6420(97)30012-8.
Çiftci F, Ûnal M, Civelek L, Sönmez M, Yildirim Ş. Clinicopathological study of lacrimal sac biopsy in dacryocystorhinostomy cases. Turkey, Istanbul: ESOPRS Scientific Symposium;1999.
Çiftci F, Ûnal M, Civelek L, Sönmez M, Yildirim Ş. Dakriyosistorinostomili olgularda gözyaşi kesesinde histopatolojik degişimler (Histopathologic changes in the lacrimal sac biopsy in dacryocystorhinostomy cases). Turk Oftalmol Gaz 2000;30:204-10.
Çiftci F, Erşanli D, Civelek L, Baloglu H, Karadayi K, Güngör A. Histopathologic changes in the lacrimal sac of dacryocystorhinostomy patients with and without silicone intubation. Ophthal Plast Reconstr Surg 2005;21(1):59-64. http://dx.doi.org/10.1097/01.IOP.0000148408.51615.FE.
Lee-Wing MW, Ashenhurst ME. Clinicopathologic analysis of 166 patients with primary acquired nasolacrimal duct obstruction. Ophthalmology 2001;108(11):2038-40.
http://dx.doi.org/10.1016/S0161-6420(01)00783-7.
DeAngelis D, Hurwitz J, Oestreicher J, Howarth D. The pathogenesis and treatment of lacrimal obstruction: The value of lacrimal sac and bone analysis. Orbit 2001;20(3):163-72.
http://dx.doi.org/10.1076/orbi.20.3.163.2626.
Bernardini FP, Moin M, Kersten RC, Reeves D, Kulwin DR. Routine histopathologic evaluation of the lacrimal sac during dacryocystorhinostomy: How useful is it? Ophthalmology 2002;109(7):1214-7. http://dx.doi.org/10.1016/S0161-6420(02)01082-5.
Yazici B, Yalçinbayir Ö, Filiz G, Sanli Ö. Eksternal dakriyosistorinostomide lakrimal kese biyopsisinin sonuçlan (External dacryocystorhinostomy lacrimal sac biopsy results). Turk Oftalmol Gaz 2002;32:649-53.
Soparkar CNS, Patrinely JR. Evaluation of the lacrimal sac. Ophthalmology 2003;110(12):2434-5.
Anderson NG, Wojno TH, Grossniklaus HE. Clinicopathologic findings from lacrimal sac biopsy specimens obtained during dacryocystorhinostomy. Ophthal Plast Reconstr Surg 2003;19(3):173-6. http://dx.doi.org/10.1097/01.IOP.0000066646.59045.5A.
Merkonidis C, Brewis C, Yung M, Nussbaumer M. Is routine biopsy of the lacrimal sac wall indicated at dacryocystorhinostomy? A prospective study and literature review. Br J Ophthalmol 2005;89(12):1589-91. http://dx.doi.org/10.1136/bjo.2005.072199.
Özgur OR, Kaplan A, Akçay L, Geçer M, Dogan OK. Histopathologic findings from lacrimal sac biopsy specimens obtained during external dacryocystorhinostomy. Turk Oftalmol Gaz 2008;38:9-13.
Kashkouli MB, Sadeghipour A, Kaghazkanani R, Bayat A, Pakdel F, Aghai GH. Pathogenesis of primary acquired nasolacrimal duct obstruction. Orbit 2010;29(1):11-5.
http://dx.doi.org/10.3109/01676830903207828.
Heindl LM, Treutlein E, Junemann AG, Kruse FE, Holbach LM. Selective lacrimal sac biopsy for external dacryocystorhinostomy: A clinical pathological study. Ophthalmologe 2010;107(12):1139-44. http://dx.doi.org/10.1007/s00347-010-2200-1.
Altan-Yaycioglu R, Canan H, Sizmaz S, Bal N, Pelit A, Akova YA. Nasolacrimal duct obstruction: Clinicopathologic analysis of 205 cases. Orbit 2010;29(5):254-8. http://dx.doi.org/10.3109/01676831003739699.
Salour H, Hatami MM, Parvin M, Ferdowsi AA, Abrishami M, Bagheri A, et al. Clinicopathological study of lacrimal sac specimens obtained during DCR. Orbit 2010;29(5):250-3. http://dx.doi.org/10.3109/01676830.2010.485720.
Knežević M, Stojković M, Jovanović M, Stanković Z, Rašić DM. A 7-year prospective study of routine histopathological evaluation of the lacrimal sac wall incisional biopsy specimens obtained during external dacryocystorhinostomy in adults and a review of the literature. Med Oncol 2012;29(1):396-400. http://dx.doi.org/10.1007/s12032-010-9810-y.
Ryan SJ, Font RL. Primary epithelial neoplasms of the lacrimal sac. Am J Ophthalmol 1973;76(1):73-88. http://dx.doi.org/10.1016/0002-9394(73)90014-7.
Ni C, D'Amico DJ, Fan CQ, Kuo PK. Tumors of the lacrimal sac: A clinicopathological analysis of 82 cases. Int Ophthalmol Clin 1982;22(1):121-40.
http://dx.doi.org/10.1097/00004397-198202210-00010.
Stefanyszyn MA, Hidayat AA, Pe'er JJ, Flanagan JC. Lacrimal sac tumors. Ophthal Plast Reconstr Surg 1994;10(3):169-84. http://dx.doi.org/10.1097/00002341-199409000-00005.
Marthin JK, Lindegaard J, Prause JU, Heegaard S. Lesions of the lacrimal drainage system: A clinicopathological study of 643 biopsy specimens of the lacrimal drainage system in Denmark 1910-1999. Acta Ophthalmol Scand 2005;83(1):94-9.
http://dx.doi.org/10.1111/j.1600-0420.2005.00383.x.
Valenzuela AA, McNab AA, Selva D, O'Donnell BA, Whitehead KJ, Sullivan TJ. Clinical features and management of tumors affecting the lacrimal drainage apparatus. Ophthal Plast Reconstr Surg 2006;22(2):96-101.
http://dx.doi.org/10.1097/01.iop.0000198457.71173.7b.
Amin RM, Hussein FA, Idriss HF, Hanafy NF, Abdallah DM. Pathological, immunohistochemical and microbiological analysis of lacrimal sac biopsies in patients with chronic dacryocystitis. Int J Ophthalmol 2013;6(6):817-26.
DOI: 10.3980/j.issn.2222-3959.2013.06.14.
Sjö LD, Ralfkiaer E, Juhl BR, Prause JU, Kivelä T, Auw‐Haedrich C, et al. Primary lymphoma of the lacrimal sac: An EORTC ophthalmic oncology task force study. Br J Ophthalmol 2006;90(8):1004-9. http://dx.doi.org/10.1136/bjo.2006.090589.
Heindl LM, Jünemann A, Kruse FE, Holbach LM. Tumors of the lacrimal drainage system. Orbit 2010;29(5):298-306. http://dx.doi.org/10.3109/01676830.2010.492887.
Mishra DK, Ali MJ, Bhargava A, Naik MN. Acute dacryocystitis as a presenting sign of chronic lymphocytic leukaemia. Clin Experiment Ophthalmol 2016;44(1):67-9.
http://dx.doi.org/10.1111/ceo.12579.
Palamar M, Midilli R, Ozsan N, Egrilmez S, Sahin F, Yagci A. Primary diffuse large B-cell lymphoma of the lacrimal sac simulating chronic dacryocystitis. Auris Nasus Larynx 2011;38(5):643-5. http://dx.doi.org/10.1016/j.anl.2011.01.012.
Litschel R, Siano M, Tasman AJ, Cogliatti S. Nasolacrimal duct obstruction caused by lymphoproliferative infiltration in the course of chronic lymphocytic leukemia. Allergy Rhinol (Providence) 2015;6(3):191-4. http://dx.doi.org/10.2500/ar.2015.6.0130.
Erickson BP, Modi YS, Ko MJ, Hussain RM, Gomez-Fernandez C, Johnson TE. Transitional cell-type papillary carcinoma of the lacrimal sac manifesting as a medial canthal skin lesion. Orbit 2014;33(5):378-81. http://dx.doi.org/10.3109/01676830.2014.894541.
Neffendorf JE, Bagdonaite L, Mudhar HS, Pearson AR. Adult alveolar rhabdomyosarcoma of the lacrimal sac. Orbit 2014;33(6):468-70.
http://dx.doi.org/10.3109/01676830.2014.950295.
Kurdi M, Allen L, Wehrli B, Chakrabarti S. Solitary fibrous tumour of the lacrimal sac presenting with recurrent dacryocystitis. Can J Ophthalmol 2014;49(5):e108-10.
http://dx.doi.org/10.1016/j.jcjo.2014.05.011.
Li YJ, Zhu SJ, Yan H, Han J, Wang D, Xu S. Primary malignant melanoma of the lacrimal sac. BMJ Case Rep 2012;2012.
Jakobiec FA, Stagner AM, Sutula FC, Freitag SK, Yoon MK. Pigmentation of the lacrimal sac epithelium. Ophthal Plast Reconstr Surg [Internet] 2015 Sep [cited: 2016 Apr]. Available from Ovid: http://journals.lww.com/op-rs/Abstract/publishahead/Pigmentation_of_the_Lacrimal_Sac_Epithelium_.98940.aspx.
Dhillon N, Kreis AJ, Madge SN. Dacryolith-induced acute dacryocystitis: A reversible cause of nasolacrimal duct obstruction. Orbit 2014;33(3):199-201.
http://dx.doi.org/10.3109/01676830.2013.871300.
Bagheri A, Rafati N, Salim RE, Yazdani S. Free-floating pyogenic granuloma of the lacrimal sac. Orbit 2014;33(2):156-8. http://dx.doi.org/10.3109/01676830.2013.853808.
Downloads
Additional Files
Published
How to Cite
Accepted 2016-07-23
Published 2017-02-21