The etiology of hypertransaminasemia in Turkish children
DOI:
https://doi.org/10.17305/bjbms.2016.982Keywords:
children, DILI, hepatitis, liver, myopathy, NAFLD, transaminases, ALT, ASTAbstract
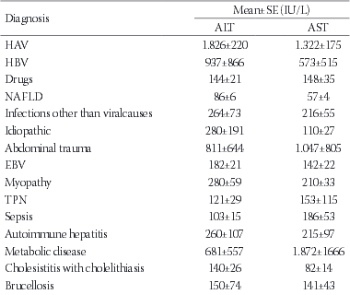
The aim of this study was to investigate the causes of elevated levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) in children. We analyzed the medical records for children aged 3 months to 18 years who presented to the hospital with ALT >45 IU/L and/or AST >50 IU/L, between 2012 and 2014, for various reasons, including those not related to liver disease. In total, 281 children met the study criteria. This group comprised of 125 (44.5%) females and 156 (55.5%) males. At the presentation, the most common patient complaint was fatigue (53.4%), while 15.7% of the patients reported no symptoms. The most common findings on the physical examination were jaundice and hepatomegaly. In 15% of the cases, the findings were normal. According to the diagnosis, the most common cause of the elevated transaminases were infections (34%), with hepatitis A virus (HAV) infection as the leading cause (18.9%). Drug-induced liver injury (DILI) was the cause in 18.1% of the cases and non-alcoholic fatty liver disease (NAFLD) in 11.1%. The highest transaminase levels were associated with HAV infection, while DILI and NAFLD caused only slightly elevated transaminases. Overall, our results show that the elevated transaminases in children are most often caused by infections, DILI, and NAFLD. In a majority of cases, elevated ALT and AST indicate liver disease, however, they could also be associated with conditions other than liver damage. Additionally, the elevated enzymes can be detected in completely healthy individuals.
Citations
Downloads
References
Schwimmer JB, Dunn W, Norman GJ, Pardee PE, Middleton MS, Kerkar N, et al. SAFETY study: alanine aminotranferase cutoff values are set too high for reliable detection of pediatric chronic liver disease. Gastroenterology 2010; 138(4):1357-1364.
http://dx.doi.org/10.1053/j.gastro.2009.12.052
Park SH, Park HY, Kang JW, Park J, Shin KJ. Aminotransferase upper reference limits and the prevalence of elevated aminotransferases in the Korean adolescent population. J Pediatr Gastroenterol Nutr 2012; 55(6):668-672.
http://dx.doi.org/10.1097/MPG.0b013e3182660669
Park HK, Hwang JS, Moon JS, Lee JA, Kim DH, Lim JS. Healthy range of serum alanine aminotransferase and its predictive power for cardiovascular risk in children and adolescents. J Pediatr Gastroenterol Nutr 2013; 56(6):686-691.
http://dx.doi.org/10.1097/MPG.0b013e31828b4e67
Giannini EG, Testa R, Savarino V. Liver enzyme alteration: a guide for clinicians. CMAJ 2005; 172(3):367–379.
http://dx.doi.org/10.1503/cmaj.1040752
Iorio R, Sepe A, Giannattasio A, Cirillo F, Vegnente A. Hypertransaminasemia in childhood as a marker of genetic liver disorders. J Gastroenterol 2005; 40(8):820-826.
http://dx.doi.org/10.1007/s00535-005-1635-7
Bugeac N, Pacht A, Mandel H, Iancu T, Tamir A, Srugo I, et al. The significance of isolated elevation of serum aminotransferases in infants and young children. Arch Dis Child 2007; 92(12):1109-1112.
http://dx.doi.org/10.1136/adc.2007.121194
Green RM, Flamm S. AGA technical review on the evaluation of liver chemistry tests. Gastroenterology 2002; 123(4):1367-1384.
http://dx.doi.org/10.1053/gast.2002.36061
Vajro P, Maddaluno S, Veropalumba C. Persistent hypertansaminasemia in asymptomatic children: a stepwise approach. World J Gastroenterol 2013; 19(18):2740-2751.
http://dx.doi.org/10.3748/wjg.v19.i18.2740
Hennes HM, Smith DS, Schneider K, Hegenbarth MA, Duma MA, Jona JZ. Elevated liver transaminase levels in children with blunt abdominal trauma: a predictor of liver injury. Pediatrics 1990; 86(1):87-90.
Sookoian S, Pirola CJ. Obstructive sleep apnea is associated with fatty liver and abnormal liver enzymes: a meta-analysis. Obes Surg 2013; 23(11):1815-1825.
http://dx.doi.org/10.1007/s11695-013-0981-4
Shen G, Zhang L, Zhang YL, Hu LP, Li MH, Lu Y, et al. Study on the etiology of acute hepatitis hospitalized patients in Beijing Ditan Hospital from 2002 to 2011 [Article in Chinese]. Zhonghua Shi Yan He Lin Chuang Bing Du XueZaZhi 2013; 27(4):266-269.
Ellis RD, Dicko A, Sagara I, Kamate B, Guindo O, Niambele MB, et al. Short report: elevated levels of alanine aminotransferase and hepatitis A in the context of a pediatric malaria vaccine trial in a village in Mali. Am J Trop Med Hyg 2008; 79(6):980-982.
Ameli M, Besharati S, Nemati K, Zamani F. Relationship between elevated liver enzyme with iron overload and viral hepatitis in thalassemia major patients in Northern Iran. Saudi Med J 2008; 29(11):1611-1615.
Akelma AZ, Kütükoğlu I, Köksal T, Çizmeci MN¸ Kanburoğlu MK, Çatal F, et al. Serum transaminase elevation in children with rotavirus gastroenteritis: seven years' experience. Scand J Infect Dis 2013; 45(5):362-367.
http://dx.doi.org/10.3109/00365548.2012.740573
Hudson OD, Nunez M, Shaibi GQ. Ethnicity and elevated liver transaminases among newly diagnosed children with type 2 diabetes. BMC Pediatr 2012; 12:174.
http://dx.doi.org/10.1186/1471-2431-12-174
M'Koma AE, Longo WE. Postoperative liver enzyme abnormalities are related to staged restorative proctocolectomy. Int J Colorectal Dis 2007; 22(3):283-288.
http://dx.doi.org/10.1007/s00384-006-0130-9
González-Contreras J, Villalobos Gámez JL, Gómez-Sánchez AI, García-Almeida JM, Enguix Armanda A, Rius Diaz F et al. Cholestasis induced by total parenteral nutrition: effects of the addition of Taurine (Tauramin®) on hepatic function parameters; possible synergistic action of structured lipids (SMOFlipid®). Nutr Hosp 2012; 27(6):1900-1907.
doi: 10.3305/nh.2012.27.6.6047
Kleiner DE, Chalasani NP, Lee WM, Fontana RJ, Bonkovsky HL, Watkins PB, et al. Drug-Induced Liver Injury Network (DILIN). Hepatic histological findings in suspected drug-induced liver injury: systematic evaluation and clinical associations. Hepatology 2014; 59(2):661-670.
http://dx.doi.org/10.1002/hep.26709
Hyun HJ, Shim JJ, Kim JW, Lee JS, Lee CK, Jang JY, et al. The prevalence of elevated alanine transaminase and its possible causes in the general Korean population. J Clin Gastroenterol 2014; 48(6):534-539. doi: 10.1097/MCG.0b013e3182a474d3
Fraser A, Longnecker MP, Lawlor DA. Prevalence of elevated alanine aminotransferase among US adolescents and associated factors: NHANES 1999-2004. Gastroenterology 2007; 133(6):1814-1820.
http://dx.doi.org/10.1053/j.gastro.2007.08.077
Purcell M, Flores YN, Zhang ZF, Denova-Gutiérrez E, Salmeron J. Prevalence and predictors of alanine aminotransferase elevation among normal weight, overweight and obese youth in Mexico. J Dig Dis 2013; 14(9):491-499.
http://dx.doi.org/10.1111/1751-2980.12072
Nobili V, Reale A, Alisi A, Morino G, Trenta I, Pisani M, et al. Elevated serum ALT in children presenting to the emergency unit: Relationship with NAFLD. Dig Liver Dis 2009; 41(10):749-752.
http://dx.doi.org/10.1016/j.dld.2009.02.048
Çeltik C, Erbaş H, Kurşun ÖS, Bostancıoğlu M, İnan M, Öner N et al. The Reasons of Elevated Serum Transaminases in Childhood [Article in Turkish]. Turk J Biochem 2008; 33(4):175–181.
Gilbert-Barness E, Barness LA, Farrell PM . Clinical Use of Pediatric Diagnostic Tests, 3rd ed. Philadelphia: Lippincott, Williams & Wilkins; 2003.
Fishbein MH, Miner M, Mogren C, Chalekson J. The spectrum of fatty liver in obese children and the relationship of serum aminotransferases to severity of steatosis. J Pediatr Gastroenterol Nutr 2003; 36(1):54–61.
http://dx.doi.org/10.1097/00005176-200301000-00012
Alvarez F, Berg PA, Bianchi FB, Bianchi L, Burroughs AK, Cancado EL, et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol 1999; 31(5):929–938.
http://dx.doi.org/10.1016/S0168-8278(99)80297-9
Tajiri K, Shimizu Y. Practical guidelines for diagnosis and early management of drug-induced liver injury. World J Gastroenterol 2008; 14(44):6774-6785.
http://dx.doi.org/10.3748/wjg.14.6774
Chalasani NP, Chalasani NP, Hayashi PH, Bonkovsky HL, Navarro VJ, Lee WM, et al . Practice Parameters Committee of the American College of Gastroenterology. ACG Clinical Guideline: the diagnosis and management of idiosyncratic drug-induced liver injury. Am J Gastroenterol 2014; 109(7):950-966. http://dx.doi.org/10.1038/ajg.2014.131
Hamaguchi M, Kojima T, Itoh Y, Harano Y, Fujii K, Nakajima T, et al. The severity of ultrasonographic findings in nonalcoholic fatty liver disease reflects the metabolic syndrome and visceral fat accumulation. Am J Gastroenterol 2007; 102(12):2708–2715.
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2016-01-30
Published 2016-02-19