Anatomical and functional outcomes of scleral buckling versus primary vitrectomy in pseudophakic retinal detachment
DOI:
https://doi.org/10.17305/bjbms.2017.1560Keywords:
Gas, pars plana vitrectomy, pseudophakic retinal detachment, scleral buckling, silicone oilAbstract
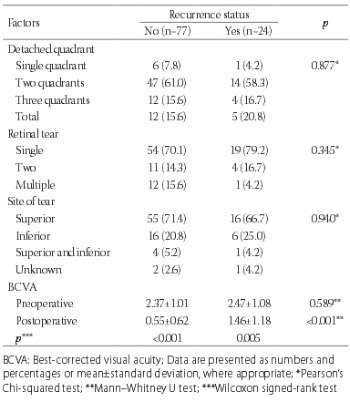
Retinal detachment is the separation of the sensory retina from the retinal pigment epithelium by subretinal fluid. There are several types of retinal re-attachment surgery, including scleral buckling (SB), pneumatic retinopexy, and vitrectomy (with or without SB). The objective of this study was to compare anatomical and visual outcomes between patients with pseudophakic rhegmatogenous retinal detachment (RRD) who underwent pars plana vitrectomy (PPV) with silicone oil (SO) or perfluoropropane (C3F8) gas tamponade and pseudophakic RRD patients who underwent SB surgery. We evaluated retrospectively 101 pseudophakic RRD patients from a single center. The patients were classified into three groups according to the surgical procedure performed: PPV + Silicone - patients who underwent PPV with SO tamponade; PPV + Gas - patients who underwent PPV with perfluoropropane gas tamponade; and SB group - patients who underwent SB surgery. The groups were compared with regard to primary and final anatomical and visual outcomes. The number of patients in PPV + Silicone, PPV + Gas, and SB group was 39 (38.6%), 32 (31.7%), and 30 (29.7%), respectively. The mean follow-up period in PPV + Silicone, PPV + Gas, and SB group was 33.95 ± 23.58, 32.62 ± 10.95, and 33.76 ± 16.62 months, respectively. No significant difference was observed between the groups neither with regard to primary and final anatomical and visual success rates nor in relation to the recurrence rate of retinal detachment. According to our anatomical and visual outcome results, either of the three methods (i.e., PPV + Silicone, PPV + Gas, or SB) can be used in the treatment of pseudophakic retinal detachment.
Citations
Downloads
References
Olsen G, Olson RJ. Update on a long-term, prospective study of capsulotomy and retinal detachment rates after cataract surgery. J Cataract Refract Surg 2000;26(7):1017-21. https://doi.org/10.1016/S0886-3350(00)00304-7.
Javitt JC, Vitale S, Canner JK. National outcomes of cataract extraction. I. Retinal detachment after inpatient surgery. Ophthalmology 1991;98(6):895-902. https://doi.org/10.1016/S0161-6420(91)32204-8.
Ah-Fat FG, Sharma MC, Majid MA, McGalliard JN, Wong D. Trends in vitreoretinal surgery at a tertiary referral center: 1987 to 1996. Br J Ophthalmol 1999;83(4):396-8. https://doi.org/10.1136/bjo.83.4.396.
Lois N, Wong D. Pseudophakic retinal detachment. Surv Ophthalmol 2003;48(5):467-87. https://doi.org/10.1016/S0039-6257(03)00083-3.
Yoshida A, Ogasawara H, Jalkh AE, Sanders RJ, McMeel JW, Schepens CL. Retinal detachment after cataract surgery. Surgical results. Ophthalmology 1992;99(3):460-5. http://dx.doi.org/10.1016/S0161-6420(92)31952-9.
Cousins S, Boniuk I, Okun E, Johnston GP, Arribas NP, Escoffery RF, et al. Pseudophakic retinal detachments in the presence of various IOL types. Ophthalmology 1986;93(9):1198-208.
https://doi.org/10.1016/S0161-6420(86)33596-6.
Yoshida A, Ogasawara H, Jalkh AE, Sanders RJ, McMeel JW, Schepens CL. Retinal detachment after cataract surgery. Predisposing factors. Ophthalmology 1992;99(3):453-9. https://doi.org/10.1016/S0161-6420(92)31953-0.
Bartz-Schmidt KU, Kirchhof B, Heimann K. Primary vitrectomy for pseudophakic retinal detachment. Br J Ophthalmol 1996;80(4):34634-9. https://doi.org/10.1136/bjo.80.4.346.
Desai UR, Strassman IB. Combined pars plana vitrectomy and scleral buckling for pseudophakic and aphakic retinal detachments in which a break is not seen preoperatively. Ophthalmic Surg Lasers 1997;28(9):718-22.
Speicher MA, Fu AD, Martin JP, von Fricken MA. Primary vitrectomy alone for repair of retinal detachments following cataract surgery. Retina 2000;20(5):459-64. https://doi.org/10.1097/00006982-200005000-00005.
Schwartz SG, Flynn HW. Primary retinal detachment: scleral buckle or pars plana vitrectomy? Curr Opin Ophthalmol 2006;17(3):245-50. https://doi.org/10.1097/01.icu.0000193097.28798.fc.
Saw SM, Gazzard G, Wagle AM, Lim J, Au Eong KG. An evidence-based analysis of surgical interventions for uncomplicated rhegmatogenous retinal detachment. Acta Ophthalmol Scand 2006;84(5):606-12.
https://doi.org/10.1111/j.1600-0420.2006.00715.x.
Benson WE, Chan P, Sharma S, Snyder WB, Bloome MA, Birch DG. Current popularity of pneumatic retinopexy. Retina 1999;19(3):238-41.
https://doi.org/10.1097/00006982-199903000-00010.
Stone TW, Mittra RA. ASRS 2013 Preferences and Trends Membership Survey. American Society of Retina Specialists; Chicago, IL, USA: 2013.
Cohen E, Zerach A, Mimouni M, Barak A. Reassessment of pneumatic retinopexy for primary treatment of rhegmatogenous retinal detachment. Clin Ophthalmol 2015;9(4):2033-7. DOI: 10.2147/OPTH.S91486.
Ling J, Noori J, Safi F, Eller AW. Pneumatic retinopexy for rhegmatogenous retinal detachment in pseudophakia. Semin Ophthalmol 2016;6:1-4. [Epub ahead of print]. https://doi.org/10.1080/08820538.2016.1190849.
Lake S, Dereklis D, Georgiadis N, Alexandridis A, Economidis P. Management of pseudophakic retinal detachment with various intraocular lens types. Ann Ophthalmol 1993;25(10):381-4.
Ho PC, Tolentino FI. Pseudophakic retinal detachment. Surgical success rate with various types of IOLs. Ophthalmology 1984;91(7):847-52.
https://doi.org/10.1016/S0161-6420(84)34227-0.
Brazitikos PD, Androudi S, Christen WG, Stangos NT. Primary pars plana vitrectomy versus scleral buckle surgery for the treatment of pseudophakic retinal detachment: a randomized clinical trial. Retina 2005;25(8):957-64.
https://doi.org/10.1097/00006982-200512000-00001.
Weichel ED, Martidis A, Fineman MS, McNamara JA, Park CH, Vander JF, et al. Pars plana vitrectomy versus combined pars plana vitrectomy-scleral buckle for primary repair of pseudophakic retinal detachment. Ophthalmology 2006;113(11):2033-40. https://doi.org/10.1016/j.ophtha.2006.05.038.
Speicher MA, Fu AD, Martin JP, von Fricken MA. Primary vitrectomy alone for repair of retinal detachments following cataract surgery. Retina 2000;20(5):459-64. https://doi.org/10.1097/00006982-200005000-00005.
Campo RV, Sipperley JO, Sneed SR, Park DW, Dugel PU, Jacobsen J, et al. Pars plana vitrectomy without scleral buckle for pseudophakic retinal detachments. Ophthalmology 1999;106(9):1811-5. https://doi.org/10.1016/S0161-6420(99)90353-6.
Martinez-Castillo V, Zapata MA, Boixadera A, Fonollosa A, García-Arumí J. Pars plana vitrectomy, laser retinopexy, and aqueous tamponade for pseudophakic rhegmatogenous retinal detachment. Ophthalmology 2007;114(2):297-302. https://doi.org/10.1016/j.ophtha.2006.07.037.
Bovey EH, Gonvers M, Sahli O. Surgical treatment of retinal detachment in pseudophakia: comparison between vitrectomy and scleral buckling. Klin Monatsbl Augenheilkd 1998;212(5):314-7. https://doi.org/10.1055/s-2008-1034893.
Le Rouic JF, Behar-Cohen F, Azan F, Bertin S, Bettembourg O, Rumen F, et al. Vitrectomy without scleral buckle versus ab-externo approach for pseudophakic retinal detachment: comparative retrospective study. [Article in French]. J Fr Ophtalmol 2002;25(3):240-5.
Sharma YR, Karunanithi S, Azad RV, Vohra R, Pal N, Singh DV, et al. Functional and anatomic outcome of scleral buckling versus primary vitrectomy in pseudophakic retinal detachment. Acta Ophthalmol Scand 2005;83(3):293-7. https://doi.org/10.1111/j.1600-0420.2005.00461.x.
Tornambe PE, Hilton GF. Pneumatic retinopexy. A multicenter randomized controlled clinical trial comparing pneumatic retinopexy with scleral buckling. The Retinal Detachment Study Group. Ophthalmology 1989;96(6):772-83. https://doi.org/10.1016/S0161-6420(89)32820-X.
Greven CM, Sanders RJ, Brown GC, Annesley WH, Sarin LK, Tasman W, et al. Pseudophakic retinal detachments. Anatomic and visual results. Ophthalmology 1992;99(2):257-62. https://doi.org/10.1016/S0161-6420(92)31983-9.
Han DP, Mohsin NC, Guse CE, Hartz A, Tarkanian CN. Comparison of pneumatic retinopexy and scleral buckling in the management of primary rhegmatogenous retinal detachment. Southern Wisconsin Pneumatic Retinopexy Study Group. Am J Ophthalmol 1998;126(5):658-68. https://doi.org/10.1016/S0002-9394(98)00181-0.
Schwartz SG, Kuhl DP, McPherson AR, Holz ER, Mieler WF. Twenty-year follow-up for scleral buckling. Arch Ophthalmol 2002;120(3):325-9. https://doi.org/10.1001/archopht.120.3.325.
Mendrinos E, Dang-Burgener NP, Stangos AN, Sommerhalder J, Pournaras CJ. Primary vitrectomy without scleral buckling for pseudophakic rhegmatogenous retinal detachment. Am J Ophthalmol 2008;145(6):1063-70. https://doi.org/10.1016/j.ajo.2008.01.018.
Arya AV, Emerson JW, Engelbert M, Hagedorn CL, Adelman RA. Surgical management of pseudophakic retinal detachments: a meta-analysis. Ophthalmology 2006;113(10):1724-33. https://doi.org/10.1016/j.ophtha.2006.05.044.
Heimann H, Bartz-Schmidt KU, Bornfeld N, Weiss C, Hilgers RD, Foerster MH, et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: a prospective randomized multicenter clinical study. Ophthalmology 2007;114(12):2142-54. https://doi.org/10.1016/j.ophtha.2007.09.013.
McCuen BW II, Azen SP, Boone DC, Lai MY, Lean JS, Linton KLP, et al. Vitrectomy with silicone oil or perfluoropropane gas in eyes with severe proliferative vitreoretinopathy: results of a randomized clinical trial. Silicone Study Report 2. Arch Ophthalmol 1992;110(6):780-92. DOI:10.1001/archopht.1992.01080180052028.
Abrams GW, Azen SP, McCuen BW 2nd, Flynn HW Jr, Lai MY, Ryan SJ. Vitrectomy with silicone oil or long-acting gas in eyes with severe proliferative vitreoretinopathy: results of additional and long-term follow-up. Silicone Study report 11. Arch Ophthalmol 1997;115(3):335-44. https://doi.org/10.1001/archopht.1997.01100150337005.
Feltgen N, Heimann H, Hoerauf H, Walter P, Hilgers RD, Heussen N. Writing group for the SPR study investigators. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment (SPR study): risk assessment of anatomical outcome. SPR study report no. 7. Acta Ophthalmol 2013;91(3):282-7. https://doi.org/10.1111/j.1755-3768.2011.02344.x.
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2016-10-31
Published 2017-02-21