Enhancing clinical decision-making in closed pelvic fractures with machine learning models
DOI:
https://doi.org/10.17305/bb.2024.10802Keywords:
Hemodynamic instability, HI, closed pelvic fracture, PF, machine learning, ML, risk prediction, clinical decision-making, mortality riskAbstract
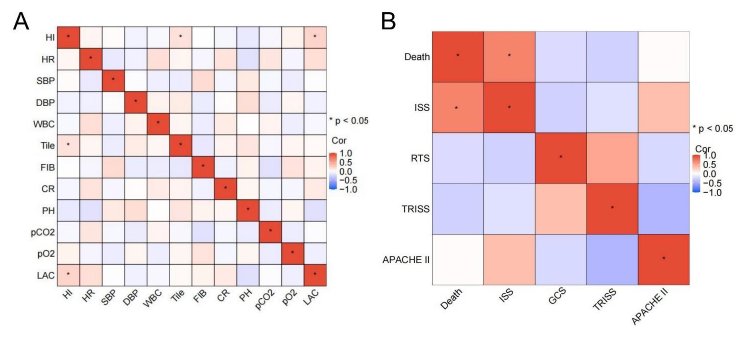
Closed pelvic fractures can lead to severe complications, including hemodynamic instability (HI) and mortality. Accurate prediction of these risks is crucial for effective clinical management. This study aimed to utilize various machine learning (ML) algorithms to predict HI and death in patients with closed pelvic fractures and identify relevant risk factors. The retrospective study included 208 patients diagnosed with pelvic fractures and admitted to Suning Traditional Chinese Medicine Hospital between 2019 and 2023. Among these, 133 cases were identified as closed PFs. Patients with closed fractures were divided into a training set (n = 115) and a test set (n = 18). The training set was further stratified into two groups based on hemodynamic stability: Group A (patients with HI) and Group B (patients with hemodynamic stability). A total of 40 clinical variables were collected, and multiple machine learning algorithms were employed to develop predictive models, including logistic regression (LR), C5.0 Decision Tree (DT), Naive Bayes (NB), support vector machine (SVM), K-nearest neighbors (KNN), random Forest (RF), and artificial neural network (ANN). Additionally, factor analysis was performed to assess the interrelationships between variables. The RF and LR algorithms outperformed traditional methods—such as central venous pressure (CVP) and intra-abdominal pressure (IAP) measurements—in predicting HI. The RF model achieved an average under the ROC (AUC) of 0.92, with an accuracy of 0.86, precision of 0.81, and an F1 score of 0.87. The LR model had an average AUC of 0.82 but shared the same accuracy, precision, and F1 score as the RF model. Key risk factors identified included TILE grade, heart rate (HR), creatinine (CR), white blood cell count (WBC), fibrinogen (FIB), and lactic acid (LAC), with LAC levels >3.7 and an injury severity score (ISS) >13 as significant predictors of HI and mortality. In conclusion, the RF and LR algorithms are effective in predicting HI and mortality risk in patients with closed PFs, enhancing clinical decision-making and improving patient outcomes.
Citations
Downloads
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2024 Dian Wang, Yongxin Li, Li Wang

This work is licensed under a Creative Commons Attribution 4.0 International License.









