HLA-DRB1*01 predicts treatment outcome in juvenile idiopathic arthritis: A retrospective-prospective cohort study
DOI:
https://doi.org/10.17305/bb.2024.11043Keywords:
Juvenile idiopathic arthritis, HLA class II alleles, treatment response, disease activity, prognostic markerAbstract
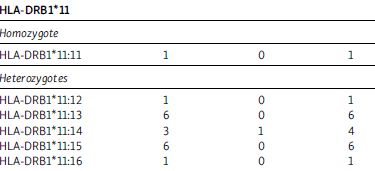
Juvenile idiopathic arthritis (JIA) is the most common chronic inflammatory autoimmune disease in childhood, significantly contributing to both short- and long-term disability. While certain human leukocyte antigen (HLA) class II alleles are known to be associated with specific subgroups of JIA, emerging evidence suggests a strong correlation between these alleles and treatment response. This study involved 143 JIA patients diagnosed according to International League of Associations for Rheumatology criteria. Each patient underwent HLA class II typing, including HLA-B27, as well as tests for rheumatoid factor (RF) and antinuclear antibodies (ANA). Comprehensive rheumatological assessments were conducted at diagnosis, with follow-ups at three and six months post-onset. After six months of methotrexate (MTX) treatment, patients were categorized as responders or non-responders. Responders achieved clinically inactive disease based on the American College of Rheumatology Provisional Criteria for Defining Clinical Inactive Disease and Clinical Remission. Non-responders, who did not reach clinically inactive disease after six months of treatment, required the addition of another non-biological disease-modifying antirheumatic drug (DMARD) or a biological DMARD. Our analysis revealed that the HLA-DRB1*01 allele is a significant prognostic marker for therapeutic response, predicting therapeutic resistance (P=0.01). The most prevalent HLA-DRB1 alleles in the treatment-resistant group were HLA-DRB1*08:11 (11.3%), HLA-DRB1*01:01 (8.5%), HLA-DRB1*01:13, HLA-DRB1*04:11 (7%), HLA-DRB1*08:13, and HLA-DRB1*08:15 (4.2%). These findings highlight the critical role of HLA class II alleles in pediatric rheumatology, particularly in relation to treatment response and disease prognosis. In the era of personalized medicine, understanding the genetic contributions to treatment response and outcomes in JIA patients is essential. A key limitation of this study was the lack of comparison of treatment responses across different JIA subtypes. Future studies should prioritize evaluating MTX efficacy within specific JIA subgroups to enable a more tailored understanding of its effectiveness.
Citations
Downloads
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2024 Adisa Čengić, Sniježana Hasanbegović, Izeta Hamza, Tarik Suljić, Velma Selmanović, Aida Đozo, Elma Fejzić, Lamija Zečević-Pašić, Nejra Džananović

This work is licensed under a Creative Commons Attribution 4.0 International License.









