FMT reduces systemic inflammatory response in severe acute pancreatitis by increasing the abundance of intestinal Bifidobacteria and fecal bacteria
DOI:
https://doi.org/10.17305/bb.2024.11445Keywords:
Severe acute pancreatitis, SAP, fecal microbial transplantation, FMT, clinical efficacyAbstract
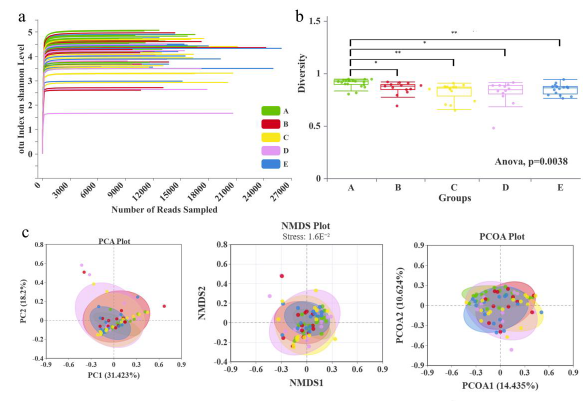
Severe acute pancreatitis (SAP) is one of the leading causes of hospital admissions for gastrointestinal diseases, with a rising incidence worldwide. Intestinal microbiota dysbiosis caused by SAP exacerbates systemic inflammatory response syndrome and organ dysfunction. Fecal microbiota transplantation (FMT) has emerged as a promising therapeutic option for gastrointestinal diseases. In this study, fecal samples from healthy, control, and FMT-treated groups were analyzed using 16S rRNA sequencing to assess microbiome abundance and diversity. Composition and functional prediction analyses were conducted to explore the mechanisms underlying FMT in SAP. FMT significantly improved clinical parameters in SAP patients, including leukocyte count, C-reactive protein (CRP), neutrophil granulocyte count, lactate dehydrogenase (LDH), and calcitonin (P < 0.05). Organ failure rates significantly increased in the control group but decreased in the FMT group after treatment (P < 0.05). Fecal microbiota sequencing revealed that FMT significantly upregulated the abundance of Bifidobacterium longum among all SAP patients (P < 0.05). Receiver operating characteristic (ROC) curve analysis indicated that Bifidobacterium longum might play a critical role in the efficacy of FMT, with an area under the curve (AUC) value of 0.84. Additionally, there was a negative correlation between Bifidobacterium longum abundance and procalcitonin (PCT) levels, as well as a negative correlation between Escherichia coli abundance and both CT and Ca values (P < 0.05). The relative abundances of Bifidobacterium longum and Escherichia coli were significantly higher in the FMT group compared to the Bifidobacterium triple viable group (P < 0.05). In conclusion, this research supports FMT as a safe and effective intervention for treating SAP patients.
Citations
Downloads
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2024 Yanning Mao, Yandong Huang, Weiwei Zhang, Huiping Liang, Fengming Liu, Qi Luo, Chunqin Xu, Yi Qin, Jiawen Liu, Shaobo Tang, Huaying Liu, Xiaolong Ge

This work is licensed under a Creative Commons Attribution 4.0 International License.









