Comparison of ProSeal laryngeal mask airway (PLMA) with cuffed and uncuffed endotracheal tubes in infants
DOI:
https://doi.org/10.17305/bjbms.2016.1219Keywords:
Infant, airway, ProSealTM laryngeal mask airway, endotracheal tubes, post-operative complicationsAbstract
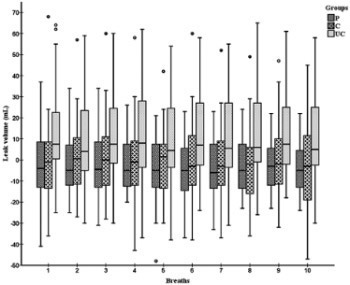
We aimed to compare cuffed and uncuffed endotracheal tubes (ETTs) with ProSealTM laryngeal mask airway (PLMA) in terms of airway security and extubation, starting out from the hypothesis that PLMA will provide alternative airway safety to the endotracheal tubes, and that airway complications will be less observed. After obtaining approval from the local Ethics Committee and parental informed consent, 120 pediatric patients 1-24 months old, American Society of Anesthesiologists physical status I-II, requiring general anesthesia for elective lower abdominal surgery, were randomized into PLMA (Group P, n = 40), cuffed ETT (Group C, n = 40), and uncuffed ETT (Group UC, n = 40) groups. The number of intubation or PLMA insertion attempts was recorded. Each patient’s epigastrium was auscultated for gastric insufflation, leak volumes and air leak fractions (leak volume/inspiratory volume) were recorded. Post-operative adverse events related to airway management were also followed up during the first post-operative hour. Demographic and surgical data were similar among the groups. There were significantly fewer airway manipulations in the Group P than in the other groups (p < 0.01), and leak volume and air leak fractions were greater in the Group UC than in the other two groups (p < 0.01). Laryngospasm was significantly lower in the Group P during extubation and within the first minute of post-extubation than in the other groups (p < 0.01). Based on this study, PLMA may be a good alternative to cuffed and uncuffed ETTs for airway management of infants due to the ease of manipulation and lower incidence of laryngospasm.
Citations
Downloads
References
. Khine HH, Corddry DH, Kettrick RG, Martin TM, McCloskey JJ, Rose JB, et al. Comparison of cuffed and uncuffed endotracheal tubes in young children during general anesthesia. Anesthesiology 1997;86(3):627-31. http://dx.doi.org/10.1097/00000542-199703000-00015.
. Ong M, Chambers NA, Hullet B, Erb TO, von Ungern-Sternberg BS. Laryngeal mask airway and tracheal tube cuff pressures in children: Are clinical endpoints valuable for guiding inflation? Anaesthesia 2008;63(7):738-44. http://dx.doi.org/10.1111/j.1365-2044.2008.05486.x.
. Al-Mazrou KA, Abdullah KM, ElGammal MS, Ansari RA, Turkistani A, Abdelmeguid ME. Laryngeal mask airway vs. Uncuffed endotracheal tube for nasal and paranasal sinus surgery: Paediatric airway protection. Eur J Anaesthesiol 2010;27(1):16-9. http://dx.doi.org/10.1097/EJA.0b013e32832c5f09.
. Goldmann K, Roettger C, Wulf H. Use of the ProSeal laryngeal mask airway for pressure-controlled ventilation with and without positive end-expiratory pressure in paediatric patients: A randomized, controlled study. Br J Anaesth 2005;95(6):831-4. http://dx.doi.org/10.1093/bja/aei246.
. Sinha A, Sharma B, Sood J. ProSeal as an alternative to endotracheal intubation in pediatric laparoscopy. Paediatr Anaesth 2007;17(4):327-32. http://dx.doi.org/10.1111/j.1460-9592.2006.02127.x.
. Cox RG, Lardner DR. Supraglottic airways in children: Past lessons, future directions. Can J Anaesth 2009;56(9):636-42. http://dx.doi.org/10.1007/s12630-009-9135-5.
. Lopez-Gil M, Brimacombe J. The ProSeal laryngeal mask airway in children. Paediatr Anaesth 2005;15(3):229-34.
http://dx.doi.org/10.1111/j.1460-9592.2005.01427.x.
. Wheeler M. ProSeal laryngeal mask airway in 120 pediatric surgical patients: A prospective evaluation of characteristics and performance. Paediatr Anaesth 2006;16(3):297-301. http://dx.doi.org/10.1111/j.1460-9592.2005.01788.x.
. Luten RC, McAllister JD. Approach to the pediatric airway. In: Walls RM, Murphy MF, editors. Manual of Emergency Airway Management. 3rd ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2008. p. 263-81.
. Lopez-Gil M, Brimacombe J, Garcia G. A randomized non-crossover study comparing the ProSeal and Classic laryngeal mask airway in anaesthetized children. Br J Anaesth 2005;95(6):827-30. http://dx.doi.org/10.1093/bja/aei234.
. Motoyama EK, Gronert BJ, Fine GF. Induction of anesthesia and maintenance of the airway in infants and children. In: Motoyama EK, Davis PJ, editors. Smith’s Anesthesia for Infants and Children. St Louis: Mosby Co; 2006. p. 336. http://dx.doi.org/10.1016/B978-032302647-5.50015-1.
. Lee KW, Templeton JJ, Dougal RM. Tracheal tube size and postintubation croup in children. Anesthesiology 1980;53:S325.
http://dx.doi.org/10.1097/00000542-198009001-00325.
. Engelhardt T, Johnston G, Kumar MM. Comparison of cuffed, uncuffed tracheal tubes and laryngeal mask airways in low flow pressure controlled ventilation in children. Paediatr Anaesth 2006;16(2):140-3.
http://dx.doi.org/10.1111/j.1460-9592.2005.01709.x.
. Brimacomb J, Keller C, Kurian S, Myles J. Reliability of epigastric auscultation to detect gastric insufflation. Br J Anaesth 2002;88(1):127-9. http://dx.doi.org/10.1093/bja/88.1.127.
. Weiss M, Dullenkopf A, Fischer JE, Keller C, Gerber AC. Prospective randomized controlled multi-centre trial of cuffed or uncuffed endotracheal tubes in small children. Br J Anaesth 2009;103(6):867-73. http://dx.doi.org/10.1093/bja/aep290.
. Devitt JH, Wenstone R, Noel AG, O'Donnell MP. The laryngeal mask airway and positive-pressure ventilation. Anesthesiology 1994;80(3):550-5. http://dx.doi.org/10.1097/00000542-199403000-00011.
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2016-06-12
Published 2016-11-10









