Influence of menopause status on T-helper cell profiles in acute myocardial infarction
DOI:
https://doi.org/10.17305/bb.2025.12354Keywords:
Myocardial infarction, T-helper cells, menopause, inflammationAbstract
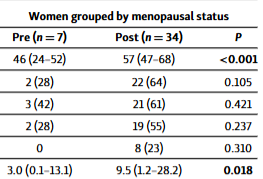
Estrogens modulate immune responses, particularly the activation and polarization of CD4+ T cells, which play key roles in cardiovascular homeostasis. This proof-of-concept study investigated the effect of menopausal status on the polarization of T-helper (Th) cells in women with acute myocardial infarction (AMI). A total of 41 female AMI patients were enrolled—seven premenopausal and 34 postmenopausal—and compared with a group of 17 male AMI patients. Flow cytometry was used to evaluate CD4+ T-cell subsets, including Th1 (T-bet+), Th2 (GATA3+), and Th17 (RORγt+) phenotypes. Serum levels of representative cytokines were also measured. Women exhibited higher numbers of circulating CD4+ T cells compared to men, with a marked shift toward the Th1 phenotype. Postmenopausal women demonstrated increased cardiovascular risk, as indicated by higher QRISK3 and GRACE scores, as well as elevated levels of C-reactive protein and cardiac troponin T compared to premenopausal women. However, menopausal status had minimal impact on Th cell polarization, as no significant differences were observed in the proportions of Th1, Th2, or Th17 subsets between premenopausal and postmenopausal women. Similarly, levels of interleukin (IL)-6, IL-1β, IL-10, tumor necrosis factor, and monocyte chemoattractant protein-1 were comparable between the two groups. This proof-of-concept study highlights sex-specific differences in immune responses and inflammatory profiles during AMI. Women exhibited a stronger polarization toward the Th1 phenotype, along with elevated markers of inflammation and myocardial injury. Notably, menopausal status did not significantly affect lymphocyte subpopulations or circulating cytokine levels.
Citations
Downloads
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Fernanda Espinosa-Bautista, Varna Ramos-Rosillo, Yadira V´ázquez-Panchos, Fernanda Bocanegra-Zamora, Héctor González-Pacheco, Mariana Patlán, Araceli Páez, Felipe Massó, Luis M Amezcua-Guerra

This work is licensed under a Creative Commons Attribution 4.0 International License.









