Prognostic impact of pan-immune inflammation value in small-cell lung cancer treated with chemoradiotherapy and prophylactic cranial irradiation
DOI:
https://doi.org/10.17305/bb.2025.12669Keywords:
Small cell lung cancer , Pan-immune inflammation value , Chemoradiotherapy, Prophylactic cranial irradiation, PrognosisAbstract
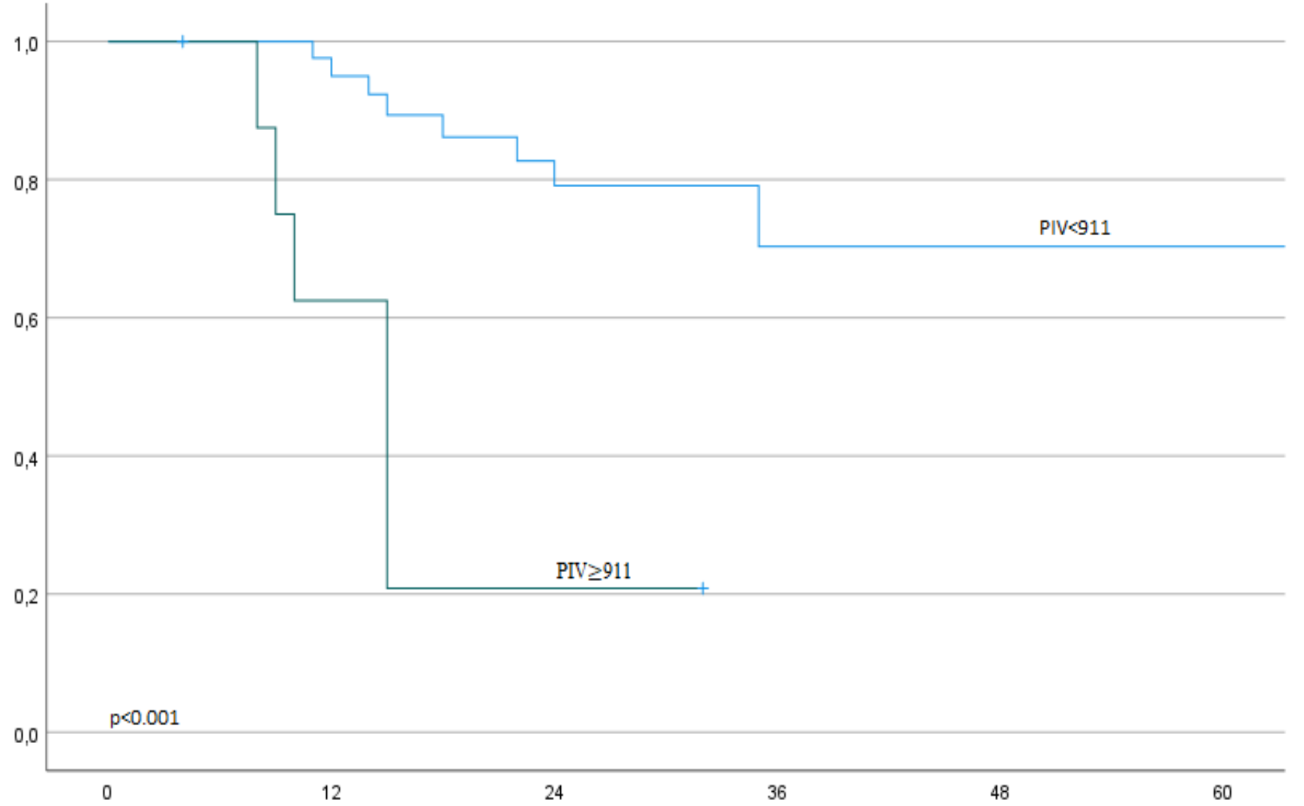
Determining prognosis is crucial for treatment selection, especially for prophylactic cranial irradiation (PCI), in patients with limited-stage small cell lung cancer (LS-SCLC). This study evaluates the prognostic value of the pan-immune inflammation value (PIV) in patients with LS-SCLC. We included patients who underwent thoracic chemoradiotherapy (TRT) and PCI at our clinic between July 2012 and April 2024. PIV was calculated as (neutrophil count × platelet count × monocyte count) / lymphocyte count. Receiver operating characteristic (ROC) curve analysis was used to determine the optimal pre-treatment PIV cut-off to divide patients into two groups. Survival outcomes between these groups were compared using Kaplan-Meier analysis and log-rank tests. Multivariate analyses were conducted using Cox regression. Fifty-nine patients were included in the study. The optimal PIV cut-off was identified as 911 (AUC: 0.60, Sensitivity: 0.31, Specificity: 0.94, J-index: 0.26). Patients were grouped based on PIV levels: low (<911) and high (≥911). Lower PIV levels were significantly associated with improved overall survival (OS) (39 months vs. 10 months, p < 0.001) and intracranial progression-free survival (ICPFS) (not reached vs. 15 months, p < 0.001). The independent prognostic value of PIV was confirmed in multivariate analyses for both OS (p < 0.001) and ICPFS (p < 0.001). These findings suggest that pre-treatment PIV is an independent prognostic marker in LS-SCLC patients undergoing TRT and PCI.
Citations
Downloads
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Aybala Nur Ucgul, Huseyin Hazir, Huseyin Bora

This work is licensed under a Creative Commons Attribution 4.0 International License.









