Procalcitonin in acute and chronic coronary syndromes: Diagnostic biomarker of coronary inflammation
DOI:
https://doi.org/10.17305/bb.2025.12915Keywords:
Procalcitonin, coronary artery disease, acute coronary syndrome, chronic coronary syndrome, inflammationAbstract
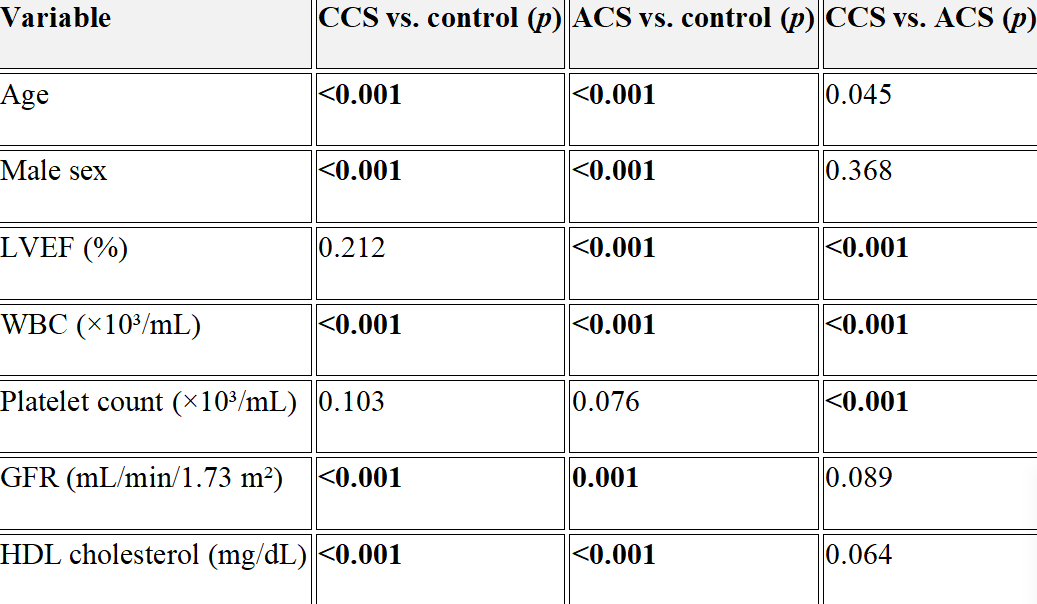
Procalcitonin (PCT) is classically a biomarker of bacterial infection, but its role in cardiovascular inflammation—particularly in coronary artery disease (CAD)—is less well defined. Evidence linking PCT with disease extent and outcomes across acute coronary syndrome (ACS) and chronic coronary syndrome (CCS) remains limited. We compared PCT levels among ACS, CCS, and angiographic controls; examined associations with inflammatory burden and anatomic complexity (SYNTAX score); and evaluated diagnostic performance and short- and intermediate-term prognostic value. In this single-center retrospective study, 477 consecutive adults undergoing diagnostic coronary angiography (December 2019–March 2020) were categorized as ACS (n=190), CCS (n=202), or controls with normal epicardial arteries (n=85). Demographic, laboratory, and angiographic data were collected. PCT was measured within 24 hours of admission. Multivariable logistic regression (using log10-transformed PCT) assessed independent associations with ACS and CCS. Correlations tested relationships with SYNTAX, C-reactive protein (CRP), and troponin-I. Receiver operating characteristic (ROC) analyses quantified discrimination. In ACS, outcomes were compared by PCT ≥0.25 ng/mL. Median PCT was higher in ACS and CCS than in controls (both p<0.001). Log10-PCT independently predicted disease presence in ACS (OR 4.30, 95% CI 2.00–9.20, p<0.001) and CCS (OR 2.81, 95% CI 1.43–5.54, p=0.003). In CCS, PCT correlated weakly but significantly with SYNTAX score (r=0.274, p=0.002); no meaningful correlations with SYNTAX, CRP, or troponin-I were observed in ACS. PCT showed moderate diagnostic accuracy (AUC 0.791 for ACS; optimal cut-off 0.25 ng/mL, sensitivity 82.4%, specificity 65.3%; and AUC 0.763 for CCS; optimal cut-off 0.30 ng/mL, sensitivity 89.4%, specificity 54.0%; all p<0.001). In ACS, PCT ≥0.25 ng/mL was not associated with higher in-hospital mortality, 1-year all-cause mortality, or major adverse cardiovascular events. PCT reflects inflammatory burden and the presence of CAD in both ACS and CCS and remains an independent predictor of disease presence, but its prognostic utility—particularly in ACS—is limited. PCT should complement, not replace, established biomarkers and anatomical scoring systems in clinical decision-making. Prospective, multicenter studies with serial PCT measurements are warranted to refine its clinical role.
Citations
Downloads
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Ozan Sakarya, Burak Toprak, Rıdvan Bora

This work is licensed under a Creative Commons Attribution 4.0 International License.









