Association between the CRP–TyG index and lupus nephritis risk
DOI:
https://doi.org/10.17305/bb.2025.13043Keywords:
C-reactive protein-triglyceride-glucose index, systemic lupus erythematosus, lupus nephritis, proteinuriaAbstract
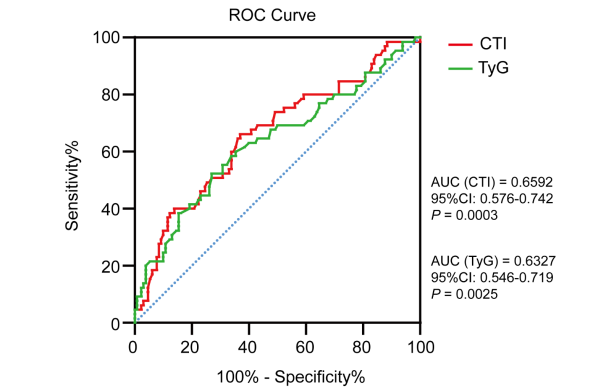
Assessment of insulin resistance is increasingly emphasized in patients with systemic lupus erythematosus (SLE) due to its significant role in predicting kidney injury and cardiovascular risk. Given that sustained inflammation is a hallmark of SLE, the novel C-reactive protein (CRP)-triglyceride-glucose (TyG) index (CTI), which comprehensively reflects insulin resistance and inflammation, has emerged as a valuable biomarker. This study aimed to investigate the association between the CTI and the risk of lupus nephritis (LN) risk and further explore its predictive potential in SLE patients. A cohort of 195 SLE patients stratified by renal involvement or CTI tertiles were included. Spearman’s correlation analysis was performed to assess the relationship between the CTI and clinical parameters of lupus activity. Logistic regression analysis was utilized to identify the association between the CTI and risk of LN. The receiver operating characteristic (ROC) curve was employed to evaluate the CTI and the TyG index in predicting LN. The results demonstrated significantly elevated CTI levels in the LN group compared to the non-LN group. Multivariate-adjusted regression analysis indicated that a unit increase in CTI corresponded to enhanced risk of LN (adjusted OR =2.062; 95% CI: 1.208 – 3.522), particularly among patients in the third tertile compared to those in the first tertile (adjusted OR = 4.368; 95% CI: 1.411 – 13.520). Subgroup analysis revealed that SLE patients with a SLEDAI-2K score greater than 6 exhibited an increased LN risk associated with higher CTI levels. ROC analysis illustrated the higher sensitivity of CTI (AUC = 0.6592; 95%CI, 0.576 – 0.742) compared to the TyG index (AUC = 0.6327; 95%CI, 0.546 – 0.719) in predicting LN risk. These findings indicate that elevated CTI is strongly associated with an increased risk of LN, suggesting its potential as a valuable predictor of LN risk in SLE patients.
Citations
Downloads
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Baozhu Liang, Ming Tang, Junqi Huang, Yingfei Li, Rongmei Liang, Zeqing Zhai, Erwei Sun

This work is licensed under a Creative Commons Attribution 4.0 International License.









