Small cell lung cancer (SCLC): At the door of targeted therapies
DOI:
https://doi.org/10.17305/bb.2025.13195Keywords:
Small-cell lung cancer, DLL3, B7-H3Abstract
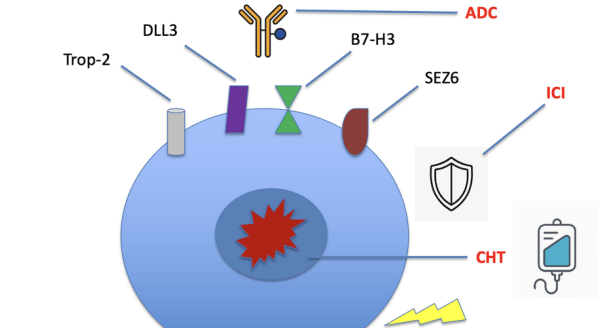
Small-cell lung cancer (SCLC) is a tobacco-associated neuroendocrine tumor comprising ~15% of lung cancers (~150,000 cases/year). For decades, outcomes stagnated: most patients present with extensive-stage disease, screening rarely detects early tumors, surgery is seldom feasible, and platinum–etoposide remained the first-line standard with median overall survival (OS) <12 months. Radiotherapy (including consolidative thoracic RT) and prophylactic cranial irradiation or MRI surveillance offered incremental gains. Two shifts have begun to change the field. First, four transcriptional subtypes (SCLC-A, -N, -P, and inflammatory SCLC-I) support a more personalized approach, with SCLC-I appearing more responsive to immune checkpoint inhibitors (ICI). Second, adding atezolizumab or durvalumab to chemotherapy in extensive-stage SCLC produced a modest median OS gain but, crucially, a tail of long-term survivors. Subsequent trials extended these advances: IMforte suggested benefit from lurbinectedin maintenance with atezolizumab in ES-SCLC, and ADRIATIC demonstrated a landmark OS improvement (~22 months) with durvalumab consolidation after concurrent chemoradiotherapy in limited-stage SCLC. Targeted strategies are now emerging. Delta-like ligand 3 (DLL3), overexpressed in >80% of SCLC, enables T-cell–redirecting therapy: the bispecific T-cell engager (BiTE®) tarlatamab improved OS to 13.6 vs 8.3 months over standard second-line chemotherapy, with manageable cytokine release syndrome and occasional ICANS. B7 homolog 3 (B7-H3, CD276), uniformly expressed across SCLC subtypes and linked to poor prognosis, is another compelling target: the antibody–drug conjugate ifinatamab deruxtecan achieved a 54.8% response rate and meaningful survival in heavily pretreated patients, earning FDA Breakthrough designation. Together, DLL3- and B7-H3–directed therapies (with additional ADCs against Trop-2 and SEZ6 in development) are redefining second-line and later care. Key next steps include optimizing sequencing/combination strategies, managing BiTE® specific toxicities, and developing predictive biomarkers. After decades of futility, SCLC is transitioning from uniform chemotherapy to a precision-medicine paradigm with cautious optimism.
Citations
Downloads
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Krešimir Tomić, Semir Vranić

This work is licensed under a Creative Commons Attribution 4.0 International License.









