CARWL score as a predictor of radiation-induced periodontitis in locally advanced head and neck cancer undergoing concurrent chemoradiotherapy
DOI:
https://doi.org/10.17305/bb.2025.13335Keywords:
C-reactive protein, serum albumin, significant weight loss, periodontitis, head and neck cancer, chemoradiotherapyAbstract
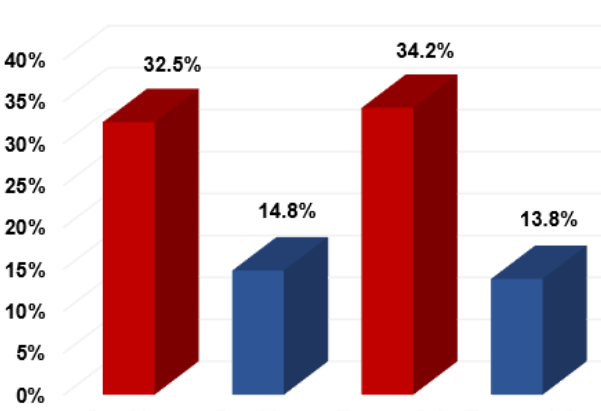
Although concurrent chemoradiotherapy (CCRT) has improved outcomes in locally advanced head and neck cancer (LA-HNC), radiation-induced periodontitis (RIP) remains an under-recognized oral toxicity with significant consequences, including tooth loss and osteoradionecrosis. This study evaluates the utility of the novel CARWL score—a combined index of the C-reactive protein-to-albumin ratio (CAR) and significant weight loss (SWL)—for stratifying the risk of RIP in LA-HNC patients without baseline periodontitis undergoing CCRT. We conducted a retrospective analysis of 67 LA-HNC patients who underwent CCRT and received detailed oral examinations before and after treatment; none had periodontitis at the initiation of CCRT. Receiver operating characteristic (ROC) curve analysis identified an optimal pretreatment CAR cutoff of 3.07, with SWL defined as greater than 5% body weight loss in the preceding six months. Based on CAR (≥3.07 vs. <3.07) and SWL (present vs. absent), patients were categorized into three CARWL groups. The primary endpoint was the association between the baseline CARWL group and the rates of RIP following CCRT. RIP was diagnosed in 17 patients (25.4%) during follow-up, with incidences increasing progressively across CARWL-0, CARWL-1, and CARWL-2 groups (11.8% vs. 20.8% vs. 38.5%; p = 0.007). In multivariable Cox proportional-hazards analysis, a higher CARWL score emerged as an independent predictor of increased RIP risk (adjusted HR = 3.64; 95% CI 1.41–9.37; p = 0.007), and supplementary logistic regression sensitivity analysis corroborated these findings (adjusted OR = 3.58; 95% CI 1.35–9.45). These findings demonstrate that the pretreatment CARWL score serves as a straightforward and readily available biomarker that effectively stratifies the risk of radiation-induced periodontitis in LA-HNC patients treated with CCRT.
Citations
Downloads
References
Kimple RJ, Harari PM. Is radiation dose reduction the right answer for HPV-positive head and neck cancer? Oral Oncol 2014;50(6):560-564. doi: https://doi.org/10.1016/j.oraloncology.2013.09.015
Chen AM, Zahra T, Daly ME, Farwell DG, Luu Q, Gandour-Edwards R, et al. Definitive radiation therapy without chemotherapy for human papillomavirus-positive head and neck cancer. Head Neck 2013;35(11):1652-6. doi: https://doi.org/10.1002/hed.23209
Koka K, Verma A, Dwarakanath BS, Papineni RVL. Technological advancements in external beam radiation therapy (EBRT): An indispensable tool for cancer treatment. Cancer Manag Res 2022;14:1421-1429. doi: https://doi.org/10.2147/CMAR.S351744
Bensadoun RJ, Patton LL, Lalla RV, Epstein JB. Oropharyngeal candidiasis in head and neck cancer patients treated with radiation: update 2011. Support Care Cancer 2011;19(6):737-44. doi: https://doi.org/10.1007/s00520-011-1154-4
Brailo V, Boras VV, Juros DV, Rogulj AA, Brzak BL, Alajbeg I. Oral Side Effects of Head and Neck Irradiation. In: Akarslan Z, ed. Head and Neck Cancer from the edited volume Diagnosis and Management of Head and Neck Cancer. London, UK: Intechopen;2017. doi: https://doi.org/10.5772/intechopen.68961
Hong CH, Napeñas JJ, Hodgson BD, Stokman MA, Mathers-Stauffers V, Elting LS, et al. A systematic review of dental disease in patients undergoing cancer therapy. Oral Care Study Group, Multi-national Association of Supportive Care in Cancer (MASCC/International Society of Oral Oncology (IS00). Support Care Cancer 2010;18(8):1007-21. doi: https://doi.org/10.1007/s00520-010-0873-2
Lalla RV, Sonis ST, Peterson DE. Management of oral mucositis in patients who have cancer. Dent Clin North Am 2008;52(1):61-77. doi: https://doi.org/10.1016/j.cden.2007.10.002
Sroussi HY, Epstein JB, Bensadoun RJ, Saunders DP, Lalla RV, Migliorati CA, et al. Common oral complications of head and neck cancer radiation therapy: mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med 2017;6(12):2918-2931. doi: https://doi.org/10.1002/cam4.1221
Bhandari S, Soni BW, Bahl A, Ghoshal S. Radiotherapy-induced oral morbidities in head and neck patients. Spec Care Dentist 2020;40(3):238-250. doi: https://doi.org/10.1111/scd.12469
Marques MAC, Dib LL. Periodontal changes in patients undergoing radiotherapy. J Periodontol 2004;75(9):1178-87. doi: https://doi.org/10.1902/jop.2004.75.9.1178
Owosho AA, Tsai CJ, Lee RS, Freymiller H, Kadempour A, Varthis S, et al. The prevalence and risk factors associated with osteoradionecrosis of the jaw in oral and oropharyngeal cancer patients treated with intensity-modulated radiation therapy (IMRT): The Memorial Sloan Kettering Cancer Center experience. Oral Oncol 2017;64:44-51. doi: https://doi.org/10.1016/j.oraloncology.2016.11.015
Huang K, Xia P, Chuang C, Weinberg V, Glastonbury CM, Eisele DW, et al. Intensity-modulated chemoradiation for treatment of stage III and IV oropharyngeal carcinoma: the University of California-San Francisco experience. Cancer 2008;113(3):497-507. doi: https://doi.org/10.1002/cncr.23578
Tobita T, Izumi K, Feinberg SE. Development of an in vitro model for radiation-induced effects on oral keratinocytes. Int J Oral Maxillofac Surg 2010;39(4):364-70. doi: https://doi.org/10.1016/j.ijom.2009.12.020
Schuurhuis JM, Stokman MA, Witjes MJH, Reintsema H, Langendijk JA, Vissink A, et al. Patients with advanced periodontal disease before intensity-modulated radiation therapy are prone to develop bone healing problems: a 2-year prospective follow-up study. Support Care Cancer 2018;26(4):1133-1142. doi: https://doi.org/10.1007/s00520-017-3934-y
Leung WK, Jin LJ, Samaranayake LP, Chiu GKC. Subgingival microbiota of shallow periodontal pockets in individuals after head and neck irradiation. Oral Microbiol Immunol 1998;13(1):1-10. doi: https://doi.org/10.1111/j.1399-302X.1998.tb00743.x
Meyle J, Chapple I. Molecular aspects of the pathogenesis of periodontitis. Periodontol 2000 2015;69(1):7-17. doi: https://doi.org/10.1111/prd.12104
Epstein JB, Robertson M, Emerton S, Phillips N, Stevenson-Moore P. Quality of life and oral function in patients treated with radiation therapy for head and neck cancer. Head Neck 2001;23(5):398-98. doi: https://doi.org/10.1002/hed.1049
Nishikawa H, Goto M, Fukunishi S, Asai A, Nishiguchi S, Higuchi K. Cancer cachexia: Its mechanism and clinical significance. Int J Mol Sci 2021;22(16):8491. doi: https://doi.org/10.3390/ijms22168491
Tasoulas J, Farquhar DR, Sheth S, Hackman T, Yarbrough WG, Agala CB, et al. Poor oral health influences head and neck cancer patient survival: an International Head and Neck Cancer Epidemiology Consortium pooled analysis. J Natl Cancer Inst 2024;116(1):105-114. doi: https://doi.org/10.1093/jnci/djad156
Sales-Peres SHC, Sales-Peres MC, Ceneviva R, Bernabe E. Weight loss after bariatric surgery and periodontal changes: a 12-month prospective study. Surg Obes Relat Dis 2017;13(4):637-642. doi: https://doi.org/10.1016/j.soard.2016.08.007
Coussens LM, Werb Z. Inflammation and Cancer. Nature 2002;420(6917):860-867. doi: https://doi.org/10.1038/nature01322
Kshirsagar AV, Craig RG, Beck JD, Moss K, Offenbacker S, Kotanko P, et al. Severe periodontitis is associated with low serum albumin among patients on maintenance hemodialysis therapy. Clin J Am Soc Nephrol 2007;2(2):239-244. doi: https://doi.org/10.2215/CJN.02420706
Martínez-García M, Hernández-Lemus E. Periodontal Inflammation and Systemic Diseases: An Overview. Front Physiol 2021;12:709438. doi: https://doi.org/10.3389/fphys.2021.709438
Sakai H, Yamada SI, Gibo T, Yoshimura N, Nishimaki F, Kondo E, et al. A retrospective analysis of the prevalence of dental diseases in patients with digestive system cancers. Medicine (Baltimore) 2019;98(13):e14771. doi: https://doi.org/10.1097/MD.0000000000014771
Song IS, Han K, Ryu JJ, Park JB. Association between underweight and tooth loss among Korean adults. Sci Rep 2017;7:41524. doi: https://doi.org/10.1038/srep41524
Topkan E, Kucuk A, Ozturk D, Ozkan EE, Besen AA, Pehlivan B, et al. Prognostic value of novel CARWL score in stage IIIC non-small-cell lung cancer patients undergoing concurrent chemoradiotherapy. Can Respir J 2024;2024:2803044. doi: https://doi.org/10.1155/2024/2803044
Somay E, Topkan E, Yilmaz B, Besen AA, Mertsoylu H, Selek U. Predicting teeth extraction after concurrent chemoradiotherapy in locally advanced nasopharyngeal cancer patients using the novel GLUCAR index. Diagnostics (Basel) 2023;13(23):3594. doi: https://doi.org/10.3390/diagnostics13233594
White SC, Pharoah MJ. Oral Radiology-E-book: Principles and Interpretation. Elsevier, St. Louis, MO, USA;2018:808-832.
World Health Organization. Oral Health Surveys: Basic Methods, 4th ed. World Health Organization, Geneva, Switzerland;1997. Volume VII, p. 66.
Silness J, Löe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 1964;22:121-135. doi: https://doi.org/10.3109/00016356408993968
Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J 1975;25(4):229-235. PMID:1058834
Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Periodontol 2018;89(Suppl 1):159-172. doi: https://doi.org/10.1002/JPER.18-0006
Caton JG, Armitage G, Berglundh T, Chapple ILC, Jepsen S, Kornman KS, et al. A new classification scheme for periodontal and peri-implant diseases and conditions-Introduction and key changes from the 1999 classification. J Clin Periodontol 2018;45(Suppl 20):1-8. doi: https://doi.org/10.1111/jcpe.12935
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 2011;12(5):489-95. doi: https://doi.org/10.1016/S1470-2045(10)70218-7
Yılmaz B, Somay E, Topkan E, Pehlivan B, Selek U. Pre-chemoradiotherapy low hemoglobin levels indicate increased osteoradionecrosis risk in locally advanced nasopharyngeal cancer patients. Eur Arch Otorhinolaryngol 2023;280(5):2575-2584. doi: https://doi.org/10.1007/s00405-023-07864-7
Grégoire V, Ang K, Budach W, Grau C, Hamoir M, Langendijk JA, et al. Delineation of the neck node levels for head and neck tumors: a 2013 update. DAHANCA, EORTC, HKNPCSG, NCIC CTG, NCRI, RTOG, TROG consensus guidelines. Radiother Oncol 2014;110(1):172-81. doi: https://doi.org/10.1016/j.radonc.2013.10.010
Borojevic T. Smoking and periodontal disease. Mater Sociomed 2012;24(4):274-6. doi: https://doi.org/10.5455/msm.2012.24.274-276
Gonçalves RB, Coletta RD, Silvério KG, Benevides L, Casati MZ, da Silva JS, et al. Impact of Smoking on Inflammation: overview of molecular mechanisms. Inflamm Res 2011;60(5):409-424. doi: https://doi.org/10.1007/s00011-011-0308-7
Irie MS, Mendes EM, Borges JS, Osuna LG, Rabelo GD, Soares PB. Periodontal therapy for patients before and after radiotherapy: A review of the literature and topics of interest for clinicians. Med Oral Patol Oral Cir Bucal 2018;23(5):e524-e530. doi: https://doi.org/10.4317/medoral.22474
Machiels JP, René Leemans C, Golusinski W, Grau C, Licitra L, Gregoire V. Squamous cell carcinoma of the oral cavity, larynx, oropharynx and hypopharynx: EHNS-ESMO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology 2020;31(11):1462-1475. doi: https://doi.org/10.1016/j.annonc.2020.07.011
Araujo TLC, Vitorino RM, Mesquita LKM, Lima AKMMN, Amaral RC, Fonseca-Silva T. Oral manifestations in patients undergoing chemotherapy. Rev Cubana Estomatol 2015;52(4):16-21.
Aradya A, Kiran PK, Raghavendia Swamy KN, Doddawad VG, Ranganatha N, Sravani K. Oral Risk Factors in Patients with Cancer Undergoing Chemotherapy- A Pilot Study. Indian J Dent Res 2024;35(2):126-130. doi: https://doi.org/10.4103/ijdr.ijdr_516_23
Mravak-Stipetic' M. Xerostomia-diagnosis and treatment. Rad514 Med Sci 2012;38:69-91.
Azher U, Shiggaon N. Oral health status of children with acute lymphoblastic leukemia undergoing chemotherapy. Indian J Dent Res 2013;24(4):523. doi: https://doi.org/10.4103/0970-9290.118371
Hancock PJ, Epstein JB, Sadler GR. Oral and dental management related to radiation therapy for head and neck cancer. J Can Dent Assoc 2003;69(9):585-90. PMID:14653934
Hommez GM, De Meerleer GO, De Neve WJ, De Moor RJ. Effect of radiation dose on the prevalence of apical periodontitis-a dosimetric analysis. Clin Oral Invest 2012;16(6):1543-1547. doi: https://doi.org/10.1007/s00784-011-0665-1
Pathomburi J, Nalampang S, Makeudom A, Klangjorhor J, Supanchart C, Krisanaprakornkit S. Effects of low-dose irradiation on human osteoblasts and periodontal ligament cells. Arch Oral Biol 2020;109:104557. doi: https://doi.org/10.1016/j.archoralbio.2019.104557
Kassim N, Sirajuddin S, Biswas S, Rafiuddin S, Apine A. Iatrogenic damage to the periodontium caused by radiation and radiotherapy. Open Dent J 2015;9:182-6. doi: https://doi.org/10.2174/1874210601509010182
Silverman S Jr, Chierici G. Radiation therapy of oral carcinoma. I. Effects on oral tissues and management of the periodontium. J Periodontol 1965;36(6):478-484. doi: https://doi.org/10.1902/jop.1965.36.6.478
Yilmaz B, Somay E, Selek U, Topkan E. Pretreatment systemic immune-inflammation index predicts needs for teeth extractions for locally advanced head and neck cancer patients undergoing concurrent chemoradiotherapy. Ther Clin Risk Manag 2021;17:1113-1121. doi: https://doi.org/10.2147/TCRM.S334556
Bansal T, Pandey A, D D, Asthana AK. C-reactive protein (CRP) and its association with periodontal disease: A brief review. J Clin Diagn Res 2014;8(7):ZE21-4. doi: https://doi.org/10.7860/JCDR/2014/8355.4646
Ebersole JL, Cappelli D. Acute-phase reactants in infections and inflammatory diseases. Periodontol 2000 2000;23:19-49. doi: https://doi.org/10.1034/j.1600-0757.2000.2230103.x
Slade GD, Offenbacher S, Beck JD, Heiss G, Pankow JS. Acute-phase inflammatory response to periodontal disease in the US population. J Dent Res 2000;79(1):49-57. doi: https://doi.org/10.1177/00220345000790010701
Noack B, Genco RJ, Trevisan M, Grossi S, Zambon JJ, De Nardin E. Periodontal infections contribute to elevated systemic C-reactive protein level. J Periodontol 2001;72(9):1221-7. doi: https://doi.org/10.1902/jop.2000.72.9.1221
Kaur N, Kaur N, Sarangal V. A study to evaluate the correlation of serum albumin levels with chronic periodontitis. Indian J Dent Res 26(1):11-14. doi: https://doi.org/10.4103/0970-9290.156788
Ogawa H, Yoshihara A, Amarasena N, Hirotomi T, Miyazaki H. Association between serum albumin and periodontal disease in community-dwelling elderly. J Clin Periodontol 2006;33(5):312-6. doi: https://doi.org/10.1111/j.1600-051X.2005.00901.x
Sheetal A, Hiremath VK, Patil AG, Sajjansetty S, Kumar SR. Malnutrition and its oral outcome: a review. J Clin Diagn Res 2013;7(1):178-80. doi: https://doi.org/10.7860/JCDR/2012/5104.2702
Ehizele AO, Ojehanon PI, Akhionbare O. Nutrition and oral health. Benin Journal of Postgraduate Medicine 2009;11(1):76-82. doi: https://doi.org/10.4314/bjpm.v11i1.48830
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2025 Sibel Bascil, Efsun Somay, Nilüfer Kılıc Durankuş, Şükran Senyürek, Düriye Ozturk, Ugur Selek, Erkan Topkan

This work is licensed under a Creative Commons Attribution 4.0 International License.









