Association of laryngopharyngeal reflux with chronic rhinosinusitis prevalence in adults: A systematic review and meta-analysis
DOI:
https://doi.org/10.17305/bb.2025.13354Keywords:
Laryngopharyngeal reflux, chronic rhinosinusitis, association, meta-analysisAbstract
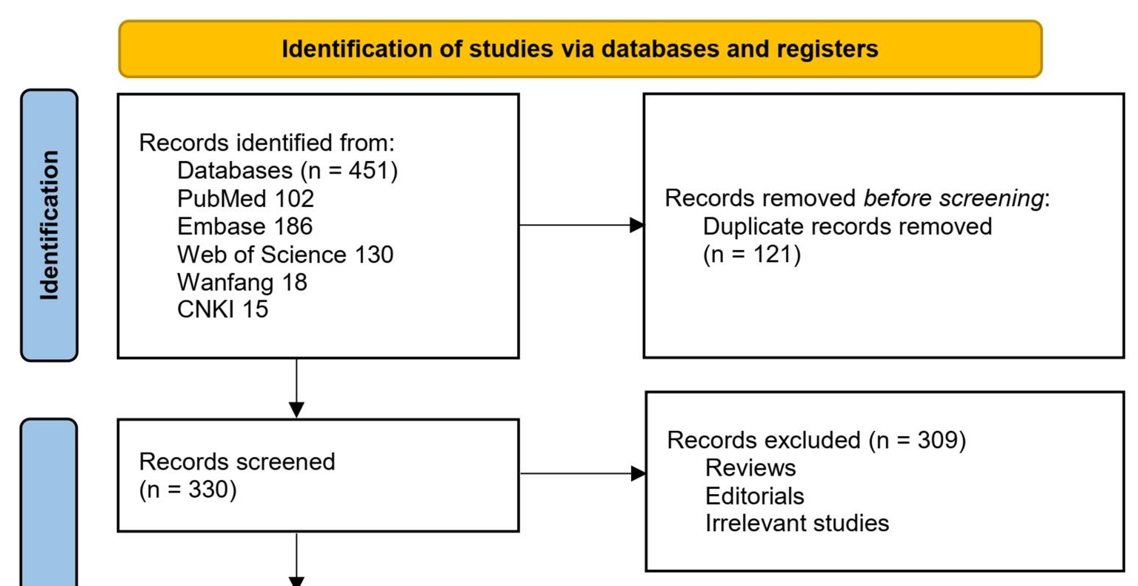
Laryngopharyngeal reflux (LPR) has been implicated in the pathogenesis of chronic rhinosinusitis (CRS), but the evidence from individual studies remains inconsistent. This meta-analysis aims to clarify the association between LPR and CRS in adults. We systematically searched PubMed, Embase, Web of Science, CNKI, and Wanfang for observational studies that evaluate the relationship between LPR and CRS in adult populations. Heterogeneity among studies was assessed using the Cochrane Q test and the I² statistic. Odds ratios (ORs) and 95% confidence intervals (CIs) were pooled using a random-effects model to account for heterogeneity. A total of eight cross- sectional studies involving 3,456 participants were included in the analysis. The results indicated a significant association between LPR and a higher prevalence of CRS in adults (OR = 4.77, 95% CI 2.51 to 9.07; p < 0.001; I² = 63%). Sensitivity analysis restricted to high-quality studies (Newcastle-Ottawa Scale score ≥ 7) produced similar results with no observed heterogeneity (OR = 5.98, 95% CI 3.60 to 9.92; I² = 0%). Exploratory subgroup analyses suggested a stronger association in studies with smaller sample sizes and when both LPR and CRS were diagnosed using objective methods. No significant evidence of publication bias was detected through Egger’s test (p = 0.35); however, this analysis was underpowered and should be interpreted cautiously in the context of the small-study effect. In conclusion, LPR may be associated with an increased prevalence of CRS in adults, especially when both conditions are diagnosed using objective criteria. Further prospective studies are needed to confirm this association and explore the underlying mechanisms.
Citations
Downloads
References
Klover CR, Gorantla VR. Chronic rhinosinusitis management: a narrative review comparing interventional treatment with osteopathic manipulation. Cureus. 2024;16(9):e70276. https://doi.org/10.7759/cureus.70276
Sedaghat AR, Phillips KM. Chronic rhinosinusitis disease control: a review of the history and the evidence. Expert Rev Clin Immunol. 2023;19(8):903–10. https://doi.org/10.1080/1744666X.2023.2229027
Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S, et al. Executive summary of EPOS 2020 including integrated care pathways. Rhinology. 2020;58(2):82–111. https://doi.org/10.4193/Rhin20.601
Min HK, Lee S, Kim S, Son Y, Park J, Kim HJ, et al. Global incidence and prevalence of chronic rhinosinusitis: a systematic review. Clin Exp Allergy. 2025;55(1):52–66. https://doi.org/10.1111/cea.14592
Choi A, Xu S, Luong AU, Wise SK. Current review of comorbidities in chronic rhinosinusitis. Curr Allergy Asthma Rep. 2024;25(1):4. https://doi.org/10.1007/s11882-024-01184-4
Kim DH, Han JS, Kim GJ, Basurrah MA, Hwang SH. Clinical predictors of polyps recurring in patients with chronic rhinosinusitis and nasal polyps: a systematic review and meta-analysis. Rhinology. 2023;61(6):482–497. https://doi.org/10.4193/Rhin23.136
Cui N, Dai T, Liu Y, Wang YY, Lin JY, Zheng QF, et al. Laryngopharyngeal reflux disease: updated examination of mechanisms, pathophysiology, treatment, and association with gastroesophageal reflux disease. World J Gastroenterol. 2024;30(16):2209–19. https://doi.org/10.3748/wjg.v30.i16.2209
Wang L, Wang G, Li L, Fan X, Liu H, Sun Z, et al. Relationship between laryngopharyngeal reflux disease and gastroesophageal reflux disease based on synchronous esophageal and oropharyngeal Dx-pH monitoring. Am J Otolaryngol. 2020;41(3):102441. https://doi.org/10.1016/j.amjoto.2020.102441
Lien HC, Lee PH, Wang CC. Diagnosis of laryngopharyngeal reflux: past, present, and future—a mini-review. Diagnostics (Basel). 2023;13(9):1643. https://doi.org/10.3390/diagnostics13091643
Samuels TL, Aoun J, Husain I, Figueredo E, Richards D, Johnston N. Advances in laryngopharyngeal reflux: etiology, diagnosis, and management. Ann N Y Acad Sci. 2024;1541(1):53–62. https://doi.org/10.1111/nyas.15242
Lechien JR, Mouawad F, Bobin F, Bartaire E, Crevier-Buchman L, Saussez S. Review of management of laryngopharyngeal reflux disease. Eur Ann Otorhinolaryngol Head Neck Dis. 2021;138(4):257–67. https://doi.org/10.1016/j.anorl.2020.11.002
Wang J, Zhao Y, Ren JJ, Lei L, Xu Y. [Laryngopharyngeal reflux and chronic rhinosinusitis]. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2016;30(20):1663–6.
Lechien JR, Ragrag K, Kasongo J, Favier V, Mayo-Yanez M, Chiesa-Estomba CM, et al. Association between Helicobacter pylori, reflux and chronic rhinosinusitis: a systematic review. Eur Arch Otorhinolaryngol. 2025 Feb 2. Online ahead of print. https://doi.org/10.1007/s00405-025-09212-3
Ulualp SO, Toohill RJ, Shaker R. Pharyngeal acid reflux in patients with single and multiple otolaryngologic disorders. Otolaryngol Head Neck Surg. 1999;121(6):725–30. https://doi.org/10.1053/hn.1999.v121.a98010
DelGaudio JM. Direct nasopharyngeal reflux of gastric acid is a contributing factor in refractory chronic rhinosinusitis. Laryngoscope. 2005;115(6):946–57. https://doi.org/10.1097/01.MLG.0000163751.00885.63
Jecker P, Orloff LA, Wohlfeil M, Mann WJ. Gastroesophageal reflux disease (GERD), extraesophageal reflux (EER) and recurrent chronic rhinosinusitis. Eur Arch Otorhinolaryngol. 2006;263(7):664–7. https://doi.org/10.1007/s00405-006-0022-1
Pasic TR, Palazzi-Churas KL, Connor NP, Cohen SB, Leverson GE. Association of extraesophageal reflux disease and sinonasal symptoms: prevalence and impact on quality of life. Laryngoscope. 2007;117(12):2218–28. https://doi.org/10.1097/MLG.0b013e31813e5fd7
Li XY, Li JR, Zhang SJ, Zhang YQ, Qi ZW, Niu RF. [A preliminary study on the relationship between laryngopharyngeal reflux and chronic rhinosinusitis]. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2017;31(23):1828–32.
Wang J, Yu Z, Ren J, Xu Y, Zhang Y, Lei L, et al. Effects of pepsin A on heat shock protein 70 response in laryngopharyngeal reflux patients with chronic rhinosinusitis. Acta Otolaryngol. 2017;137(12):1253–9. https://doi.org/10.1080/00016489.2017.1360515
Bergqvist J, Bove M, Andersson A, Scholer L, Hellgren J. Dose-dependent relationship between nocturnal gastroesophageal reflux and chronic rhinosinusitis in a middle-aged population: results from the SCAPIS pilot. Rhinology. 2023;61(2):118– 23. https://doi.org/10.4193/Rhin22.297
Shen X, Zhang Z, Wu Y, Li Y, Li H, He J, et al. Association of laryngopharyngeal reflux disease and refractory chronic rhinosinusitis. Ear Nose Throat J. 2025;104(5):NP308–NP313. https://doi.org/10.1177/01455613221112355
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. https://doi.org/10.1136/bmj.n160
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane handbook for systematic reviews of interventions. Version 6.2. The Cochrane Collaboration. 2021. www.training.cochrane.org/handbook
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2010. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Herzog R, Álvarez-Pasquin MJ, Díaz C, Del Barrio JL, Estrada JM, Gil Á. Are healthcare workers' intentions to vaccinate related to their knowledge, beliefs and attitudes? A systematic review. BMC Public Health. 2013;13:154. https://doi.org/10.1186/1471-2458-13-154
Kim K, Shin S, Kim S, Lee E. The relation between eHealth literacy and health- related behaviors: systematic review and meta-analysis. J Med Internet Res. 2023;25:e40778. https://doi.org/10.2196/40778
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. https://doi.org/10.1002/sim.1186
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. https://doi.org/10.1136/bmj.315.7109.629
Aldajani A, Alhussain F, Mesallam T, AbaAlkhail M, Alojayri R, Bassam H, et al. Association between chronic rhinosinusitis and reflux diseases in adults: a systematic review and meta-analysis. Am J Rhinol Allergy. 2024;38(1):47–59. https://doi.org/10.1177/19458924231210028
Chen G, Guo W, Liu S, Wang Y, Zhang X. Causal analysis between gastroesophageal reflux disease and chronic rhinosinusitis. Eur Arch Otorhinolaryngol. 2024;281(4):1819–25. https://doi.org/10.1007/s00405-023-08350-w
Lechien JR, Saussez S, Hopkins C. Association between laryngopharyngeal reflux, gastroesophageal reflux and recalcitrant chronic rhinosinusitis: a systematic review. Clin Otolaryngol. 2023;48(4):501–14. https://doi.org/10.1111/coa.14047
Chen S, Wang M, Zhang S, Huang X, Sui X, Li D, et al. The complexity of mucosal damage in gastroesophageal airway reflux disease: a molecular perspective. Gastroenterology & Endoscopy. 2025;3(1):39–46. https://doi.org/10.1016/j.gande.2024.12.003
Tack J. Review article: the role of bile and pepsin in the pathophysiology and treatment of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2006;24(Suppl 2):10–6. https://doi.org/10.1111/j.1365-2036.2006.03040.x
Chen X, Oshima T, Shan J, Fukui H, Watari J, Miwa H. Bile salts disrupt human esophageal squamous epithelial barrier function by modulating tight junction proteins. Am J Physiol Gastrointest Liver Physiol. 2012;303(2):G199–208. https://doi.org/10.1152/ajpgi.00454.2011
Johnston N, Yan JC, Hoekzema CR, Samuels TL, Stoner GD, Blumin JH, et al. Pepsin promotes proliferation of laryngeal and pharyngeal epithelial cells. Laryngoscope. 2012;122(6):1317–25. https://doi.org/10.1002/lary.23307
Sun Y-G, Zhang L-Y. Chronic rhinosinusitis, asthma, and gastroesophageal reflux: epidemiology, pathophysiology, and comorbidity. Allergy Medicine. 2025;3:100036. https://doi.org/10.1016/j.allmed.2025.100036
Sella GCP, Tamashiro E, Anselmo-Lima WT, Valera FCP. Relation between chronic rhinosinusitis and gastroesophageal reflux in adults: systematic review. Braz J Otorhinolaryngol. 2017;83(3):356–63. https://doi.org/10.1016/j.bjorl.2016.05.012
Anzić SA, Turkalj M, Župan A, Labor M, Plavec D, Baudoin T. Eight weeks of omeprazole 20 mg significantly reduces both laryngopharyngeal reflux and comorbid chronic rhinosinusitis signs and symptoms: randomised, double-blind, placebo- controlled trial. Clin Otolaryngol. 2018;43(2):496–501. https://doi.org/10.1111/coa.13005
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2025 Jingda Xu, Min Chen, Gang Chen, Ting Lou, Long Xu

This work is licensed under a Creative Commons Attribution 4.0 International License.









