Prediabetes and cataract risk in adults: A systematic review and meta-analysis
DOI:
https://doi.org/10.17305/bb.2026.13506Keywords:
Prediabetes, hyperglycemia, cataract, association, meta-analysisAbstract
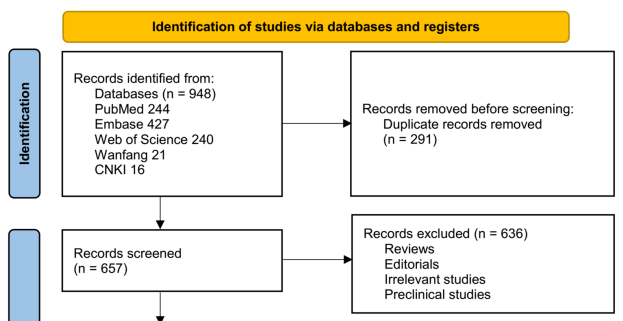
Prediabetes, characterized by impaired fasting glucose (IFG), impaired glucose tolerance (IGT), or mildly elevated glycated hemoglobin (HbA1c), represents an intermediate metabolic state potentially contributing to cataract formation. However, the existing evidence for this association remains inconsistent. This meta-analysis aims to elucidate the relationship between prediabetes and cataract in adults. A systematic search was conducted across PubMed, Embase, Web of Science, CNKI, and Wanfang for observational studies assessing the association between prediabetes and cataracts in adults. Pooled odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using random-effects models to account for heterogeneity. Subgroup analyses were performed based on study design, geographic region, diagnostic criteria for prediabetes, and covariate adjustment. Eight observational studies involving 22,342 participants were included in the analysis. Of these, 5,305 participants (23.7%) had prediabetes, and 7,625 participants (34.1%) had cataracts. Pooled results indicated that prediabetes was associated with a 34% increased odds of cataract compared to individuals with normoglycemia (OR = 1.34, 95% CI 1.11–1.61; p = 0.002; I² = 50%). Sensitivity analyses restricted to high-quality studies (NOS ≥ 7) produced consistent results (OR = 1.29, 95% CI 1.09–1.53; I² = 43%). The association remained significant across subgroups defined by geographic region, mean age, sex, diagnostic criteria for prediabetes, analytical models, and adjustment for sun exposure (all p > 0.05 for subgroup differences). In conclusion, this meta-analysis demonstrates a significant association between prediabetes and cataracts in adults. Given that most included studies were cross-sectional, these findings suggest a potential link rather than a causal relationship, highlighting the need for prospective research to clarify temporal relationships and underlying mechanisms.
Citations
Downloads
References
Chen SP, Woreta F, Chang DF. Cataracts: A Review. JAMA. 2025;333(23):2093–103.
https://doi.org/10.1001/jama.2025.1597
Wang D, Tang T, Li P, Zhao J, Shen B, Zhang M. The global burden of cataracts and its attributable risk factors in 204 countries and territories: a systematic analysis of the global burden of disease study. Front Public Health. 2024;12:1366677.
https://doi.org/10.3389/fpubh.2024.1366677
Wan Z, Bai J, Wang W, Peng Q. Global, regional, and national burden of cataract among older adults from 1990 to 2021: a comprehensive analysis based on the global burden of disease study 2021. Front Med (Lausanne). 2025;12:1679828.
https://doi.org/10.3389/fmed.2025.1679828
Flessa S. Cataract Surgery in Low-Income Countries: A Good Deal! Healthcare (Basel). 2022;10(12).
https://doi.org/10.3390/healthcare10122580
Cicinelli MV, Buchan JC, Nicholson M, Varadaraj V, Khanna RC. Cataracts. Lancet. 2023;401(10374):377–89.
https://doi.org/10.1016/S0140-6736(22)01839-6
Ang MJ, Afshari NA. Cataract and systemic disease: A review. Clin Exp Ophthalmol. 2021;49(2):118–27.
https://doi.org/10.1111/ceo.13892
Mrugacz M, Pony-Uram M, Bryl A, Zorena K. Current Approach to the Pathogenesis of Diabetic Cataracts. Int J Mol Sci. 2023;24(7).
https://doi.org/10.3390/ijms24076317
Zarei-Ghanavati S, Hadi Y, Habibi A, Ashraf Khorasani M, Yoo SH. Cataract and diabetes: review of the literature. J Cataract Refract Surg. 2024;50(12):1275–83.
https://doi.org/10.1097/j.jcrs.0000000000001547
Drinkwater JJ, Davis WA, Davis TME. A systematic review of risk factors for cataract in type 2 diabetes. Diabetes Metab Res Rev. 2019;35(1):e3073.
https://doi.org/10.1002/dmrr.3073
Echouffo-Tcheugui JB, Perreault L, Ji L, Dagogo-Jack S. Diagnosis and Management of Prediabetes: A Review. JAMA. 2023;329(14):1206–16.
https://doi.org/10.1001/jama.2023.4063
Echouffo-Tcheugui JB, Selvin E. Prediabetes and What It Means: The Epidemiological Evidence. Annu Rev Public Health. 2021;42:59–77.
https://doi.org/10.1146/annurev-publhealth-090419-102644
Schlesinger S, Neuenschwander M, Barbaresko J, Lang A, Maalmi H, Rathmann W, et al. Prediabetes and risk of mortality, diabetes-related complications and comorbidities: umbrella review of meta-analyses of prospective studies. Diabetologia. 2022;65(2):275–85.
https://doi.org/10.1007/s00125-021-05592-3
Karasik A, Modan M, Halkin H, Treister G, Fuchs Z, Lusky A. Senile cataract and glucose intolerance: the Israel Study of glucose Intolerance Obesity and Hypertension (The Israel GOH Study). Diabetes Care. 1984;7(1):52–6.
https://doi.org/10.2337/diacare.7.1.52
Rowe NG, Mitchell PG, Cumming RG, Wang JJ. Diabetes, fasting blood glucose and age-related cataract: the Blue Mountains Eye Study. Ophthalmic Epidemiol. 2000;7(2):103–14.
https://doi.org/10.1076/0928-6586(200006)721-ZFT103
Paunksnis A, Bojarskiene F, Cimbalas A, Cerniauskiene LR, Luksiene DI, Tamosiunas A. Relation between cataract and metabolic syndrome and its components. Eur J Ophthalmol. 2007;17(4):605–14.
https://doi.org/10.1177/112067210701700420
Tan JS, Wang JJ, Mitchell P. Influence of diabetes and cardiovascular disease on the long-term incidence of cataract: the Blue Mountains eye study. Ophthalmic Epidemiol. 2008;15(5):317–27.
https://doi.org/10.1080/09286580802105806
Sabanayagam C, Wang JJ, Mitchell P, Tan AG, Tai ES, Aung T, et al. Metabolic syndrome components and age-related cataract: the Singapore Malay eye study. Invest Ophthalmol Vis Sci. 2011;52(5):2397–404.
https://doi.org/10.1167/iovs.10-6373
Jiang TX, Zhai SN, Yan J, Li Y, Lu ZQ. Association between hyperlipidemia, diabetes and age-related cataract. Int Eye Sci. 2012;12(11):2098–101.
Park YH, Shin JA, Han K, Yim HW, Lee WC, Park YM. Gender difference in the association of metabolic syndrome and its components with age-related cataract: the Korea National Health and Nutrition Examination Survey 2008–2010. PLoS One. 2014;9(1):e85068.
https://doi.org/10.1371/journal.pone.0085068
Sokolowska A, Piatkiewicz P. The evaluation of ocular changes in prediabetic individuals. Clin Diabetol. 2017;6(1):8–16.
https://doi.org/10.5603/DK.2017.0003
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
https://doi.org/10.1136/bmj.n71
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.2. The Cochrane Collaboration. 2021.
www.training.cochrane.org/handbook.
Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2010.
http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280(19):1690–1.
https://doi.org/10.1001/jama.280.19.1690
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
https://doi.org/10.1002/sim.1186
Marušić MF, Fidahić M, Cepeha CM, Farcaș LG, Tseke A, Puljak L. Methodological tools and sensitivity analysis for assessing quality or risk of bias used in systematic reviews published in the high-impact anesthesiology journals. BMC Med Res Methodol. 2020;20(1):121.
https://doi.org/10.1186/s12874-020-00966-4
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
https://doi.org/10.1136/bmj.315.7109.629
Chen KY, Chan HC, Chan CM. How does diabetes shape the landscape of cataract development and surgical success? a systematic review and meta-analysis. Endocrine. 2025;90(2):404–19.
https://doi.org/10.1007/s12020-025-04374-w
Guo Z, Ma X, Zhang RX, Yan H. Oxidative stress, epigenetic regulation and pathological processes of lens epithelial cells underlying diabetic cataract. Adv Ophthalmol Pract Res. 2023;3(4):180–6.
https://doi.org/10.1016/j.aopr.2023.10.001
Ranaei Pirmardan E, Zhang Y, Barakat A, Naseri M, Russmann C, Hafezi-Moghadam A. Pre-hyperglycemia immune cell trafficking underlies subclinical diabetic cataractogenesis. J Biomed Sci. 2023;30(1):6.
https://doi.org/10.1186/s12929-023-00895-6
Zeinali Nia E, Najjar Sadeghi R, Ebadi M, Faghihi M. ERK1/2 gene expression and hypomethylation of Alu and LINE1 elements in patients with type 2 diabetes with and without cataract: Impact of hyperglycemia-induced oxidative stress. J Diabetes Investig. 2025;16(4):689–706.
https://doi.org/10.1111/jdi.14405
Khalid M, Petroianu G, Adem A. Advanced Glycation End Products and Diabetes Mellitus: Mechanisms and Perspectives. Biomolecules. 2022;12(4).
https://doi.org/10.3390/biom12040542
Wang S, Meng L, Yang H. The effects of L-tartaric acid on diabetic cataracts through modulation of oxidative stress and inflammation in diabetic rats. BMC Ophthalmol. 2025;25(1):615.
https://doi.org/10.1186/s12886-025-04409-w
Reddy VS, Reddy GB. Role of crystallins in diabetic complications. Biochim Biophys Acta. 2016;1860(1 Pt B):269–77.
https://doi.org/10.1016/j.bbagen.2015.05.009
Liu C, Zhang Y, Cao X, Chen Z. Association between metabolic syndrome and cataract: a meta-analysis. Eye (Lond). 2025;39(13):2555–64.
https://doi.org/10.1038/s41433-025-03910-2
Klein BE, Klein R, Lee KE, Knudtson MD, Tsai MY. Markers of inflammation, vascular endothelial dysfunction, and age-related cataract. Am J Ophthalmol. 2006;141(1):116–22.
https://doi.org/10.1016/j.ajo.2005.08.021
Savitz DA, Wellenius GA. Can Cross-Sectional Studies Contribute to Causal Inference? It Depends. Am J Epidemiol. 2023;192(4):514–6.
Downloads
Published
Issue
Section
Categories
License
Copyright (c) 2026 Linping Xue, Haisong Feng, Beibei Zhang, Dongmei Zuo

This work is licensed under a Creative Commons Attribution 4.0 International License.









