HALP score outperforms systemic inflammatory biomarkers for prognosis in locally advanced rectal cancer
DOI:
https://doi.org/10.17305/bb.2026.13845Keywords:
Locally advanced rectal cancer, inflammation, biomarker, prognosisAbstract
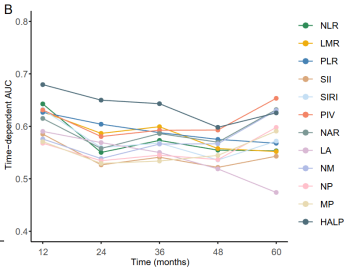
The prognostic value of systemic inflammatory and nutritional biomarkers in patients with locally advanced rectal cancer (LARC) remains inadequately defined. This multicenter retrospective study comprehensively assessed the prognostic performance of twelve inflammation-based indices, aiming to identify the most informative biomarker for patients undergoing neoadjuvant chemoradiotherapy followed by surgery. We analyzed data from 427 patients with stage II–III LARC treated at three medical centers between 2010 and 2021. Twelve biomarkers, derived from routine pretreatment blood parameters—including hemoglobin, albumin, neutrophils, lymphocytes, monocytes, and platelets—were evaluated for their association with overall survival (OS) and disease-free survival (DFS). The prognostic performance was measured using the concordance index (C-index), time-dependent area under the receiver operating characteristic curve (time-AUC), and Brier score. Among the evaluated biomarkers, the hemoglobin–albumin–lymphocyte–platelet (HALP) score exhibited robust and consistent prognostic performance. For OS, HALP achieved a C-index of 0.687 and a time-AUC of 0.668, along with the lowest Brier score (0.134); similar results were observed for DFS (C-index 0.675, time-AUC 0.665). Patients with low HALP scores had significantly worse OS and DFS compared to those with high HALP scores. Multivariate Cox regression analysis confirmed low HALP as an independent risk factor for OS (HR = 3.937, 95% CI: 2.445-6.329; p < 0.001) and DFS (HR = 2.212, 95% CI: 1.577-3.096; p < 0.001). Nomograms integrating HALP with key clinicopathological variables provided incremental prognostic value, demonstrating good discrimination and calibration at 12, 36, and 60 months. These findings indicate that HALP is a simple and cost-effective biomarker for prognostic stratification in LARC.
Citations
Downloads
References
Filho AM, Laversanne M, Ferlay J, Colombet M, Piñeros M, Znaor A, et al. The GLOBOCAN 2022 cancer estimates: Data sources, methods, and a snapshot of the cancer burden worldwide. Int J Cancer. 2025;156:1336–46.
https://doi.org/10.1002/ijc.35278
Rodet N, Zahed H, Colombet M, Bray F, McCormack V. Understanding age and sex differentials in cancer incidence and mortality: An international population-based study. Int J Cancer. 2025.
https://doi.org/10.1002/ijc.70244
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
https://doi.org/10.3322/caac.21492
Han B, Zheng R, Zeng H, Wang S, Sun K, Chen R, et al. Cancer incidence and mortality in China, 2022. J Natl Cancer Cent. 2024;4:47–53.
https://doi.org/10.1016/j.jncc.2024.01.006
Lin W, Li C, Clement EA, Brown CJ, Raval MJ, Karimuddin AA, et al. Surgical outcomes in total neoadjuvant therapy for rectal cancer versus standard long-course chemoradiation: A systematic review and meta-analysis of randomized controlled trials. Ann Surg. 2024;279:620–30.
https://doi.org/10.1097/SLA.0000000000006161
Crusz SM, Balkwill FR. Inflammation and cancer: advances and new agents. Nat Rev Clin Oncol. 2015;12:584–96.
https://doi.org/10.1038/nrclinonc.2015.105
Shen P, Xu Y, Zhu J, Qian D, Yang B, Mao Y, et al. Predictive and prognostic value of preoperative pan-immune-inflammation value in patients with locally advanced rectal cancer. Biomol Biomed. 2025;25:1000–8.
https://doi.org/10.17305/bb.2024.10658
Li B, Han J, Wang F, Yu B, Wang G, Yang F. Factors affecting survival prognosis of patients with rectal cancer after neoadjuvant chemoradiotherapy. Front Oncol. 2025;15:1562634.
https://doi.org/10.3389/fonc.2025.1562634
Bonilla-Cozar MA, Garcia-Leon A, Garcia-Sanchez CJ, Reyes-Diaz ML, Ramallo-Solis I, De la Portilla F, et al. Immunomarkers could predict overall survival and disease-free survival after neoadjuvant therapy and surgery due to locally advanced rectal cancer. Cir Esp (Engl Ed). 2025;103:800199.
https://doi.org/10.1016/j.ciresp.2025.800199
Gawiński C, Mróz A, Roszkowska-Purska K, Sosnowska I, Derezińska-Wołek E, Michalski W, et al. A prospective study on the roles of the lymphocyte-to-monocyte ratio (LMR), neutrophil-to-lymphocyte ratio (NLR), and platelet-to-lymphocyte ratio (PLR) in patients with locally advanced rectal cancer. Biomedicines. 2023;11:3048.
https://doi.org/10.3390/biomedicines11113048
Duque-Santana V, López-Campos F, Martin-Martin M, Valero M, Zafra-Martín J, Couñago F, et al. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio as prognostic factors in locally advanced rectal cancer. Oncology. 2023;101:349–57.
https://doi.org/10.1159/000526450
Chiloiro G, Romano A, Mariani S, Macchia G, Giannarelli D, Caravatta L, et al. Predictive and prognostic value of inflammatory markers in locally advanced rectal cancer (PILLAR) – A multicentric analysis by the Italian Association of Radiotherapy and Clinical Oncology (AIRO) Gastrointestinal Study Group. Clin Transl Radiat Oncol. 2023;39:100579.
https://doi.org/10.1016/j.ctro.2023.100579
Ding Y, Liu Z, Li J, Niu W, Li C, Yu B. Predictive effect of the systemic inflammation response index (SIRI) on the efficacy and prognosis of neoadjuvant chemoradiotherapy in patients with locally advanced rectal cancer. BMC Surg. 2024;24:89.
https://doi.org/10.1186/s12893-024-02384-5
Tawfik B, Mokdad AA, Patel PM, Li HC, Huerta S. The neutrophil to albumin ratio as a predictor of pathological complete response in rectal cancer patients following neoadjuvant chemoradiation. Anticancer Drugs. 2016;27(9):879–83.
https://doi.org/10.1097/CAD.0000000000000411
Yordanagil M, Bakir H, Güler Avci G, Yildirim M, Ozkan N, Ismail O. Do haematological parameters such as HALP and lymphocyte to C-reactive protein ratio predict tumor response to neoadjuvant chemoradiotherapy in locally advanced rectal cancer? Pol Przegl Chir. 2022;95:1–5.
https://doi.org/10.5604/01.3001.0016.0959
Bardakçı O, Çetinkaya G. The effectiveness of the hemoglobin, albumin, lymphocyte, and platelet (HALP) score in predicting lymph node metastasis in radiologically n0 locally advanced upper rectal cancer. Front Oncol. 2025;15:1579581.
https://doi.org/10.3389/fonc.2025.1579581
Xu H, Zheng X, Ai J, Yang L. Hemoglobin, albumin, lymphocyte, and platelet (HALP) score and cancer prognosis: A systematic review and meta-analysis of 13,110 patients. Int Immunopharmacol. 2023;114:109496.
https://doi.org/10.1016/j.intimp.2022.109496
Li J, Zheng J, Wang P, Lv D. Prognostic significance of hemoglobin, albumin, lymphocyte and platelet score in solid tumors: a pooled study. Front Immunol. 2024;15:1483855.
https://doi.org/10.3389/fimmu.2024.1483855
Farag CM, Antar R, Akosman S, Ng M, Whalen MJ. What is hemoglobin, albumin, lymphocyte, platelet (HALP) score? A comprehensive literature review of HALP's prognostic ability in different cancer types. Oncotarget. 2023;14:153–72.
https://doi.org/10.18632/oncotarget.28367
Zhang M, Xie C, Liu S, Fan H, Li Z, Tong X. The prognostic value of the hemoglobin, albumin, lymphocyte, and platelet (HALP) score in lung cancer: A systematic review and meta-analysis. J Clin Med. 2025;14:5701.
https://doi.org/10.3390/jcm14165701
Qian C, Liu J, Meng C, Cheng J, Wu B, Liao J. The significant prognostic value of the hemoglobin, albumin, lymphocyte, and platelet (HALP) score in digestive system cancers: a systematic review and meta-analysis. BMC Cancer. 2025;25:1577.
https://doi.org/10.1186/s12885-025-15068-x
Duzkopru Y, Kocanoglu A, Dogan O, Sahinli H, Cilbir E, Altinbas M. Hemoglobin, albumin, lymphocyte, and platelet score as a predictor of prognosis in metastatic gastric cancer. World J Gastrointest Oncol. 2023;15:1626–35.
https://doi.org/10.4251/wjgo.v15.i9.1626
Xie H, Wei L, Tang S, Gan J. Hemoglobin-albumin-lymphocyte-platelet score as an integrative biomarker for prognosis and sarcopenia in colorectal cancer. J Inflamm Res. 2025;18:14709–20.
https://doi.org/10.2147/JIR.S531116
Liu Q, Xie H, Cheng W, Liu T, Liu C, Zhang H, et al. The preoperative hemoglobin, albumin, lymphocyte, and platelet score (HALP) as a prognostic indicator in patients with non-small cell lung cancer. Front Nutr. 2024;11:1428950.
https://doi.org/10.3389/fnut.2024.1428950
Jiang T, Sun H, Xue S, Xu T, Xia W, Wang Y, et al. Prognostic significance of hemoglobin, albumin, lymphocyte, and platelet (HALP) score in breast cancer: a propensity score-matching study. Cancer Cell Int. 2024;24:230.
https://doi.org/10.1186/s12935-024-03419-w
Yamamoto S, Aoyama T, Maezawa Y, Hashimoto I, Esashi R, Kazama K, et al. The hemoglobin, albumin, lymphocyte and platelet (HALP) score as an independent prognostic factor for esophageal cancer patients who received curative treatment. In Vivo. 2025;39:885–93.
https://doi.org/10.21873/invivo.13892
Liu H, Zou Q, Zhang H, Ma X. Development of a prediction model based on hemoglobin, albumin, lymphocyte count, and platelet-score for lymph node metastasis in rectal cancer. Eur J Cancer Prev. 2026;35:29–37.
https://doi.org/10.1097/CEJ.0000000000000954
Wang T, Tao Y, Gan G, Chen L, Xu Y, Sun F, Xu X. Application of high-dose-rate endorectal brachytherapy in the treatment of locally advanced rectal cancer. Precis Radiat Oncol. 2025;9(2):133–142.
https://doi.org/10.1002/pro6.70004
Meng K, Lu H. Clinical application of high-LET radiotherapy combined with immunotherapy in malignant tumors. Precis Radiat Oncol. 2024;8(1):42–46.
https://doi.org/10.1002/pro6.1225
Mulita F, Liolis E, Akinosoglou K, Tchabashvili L, Maroulis I, Kaplanis C, et al. Postoperative sepsis after colorectal surgery: a prospective single-center observational study and review of the literature. Prz Gastroenterol. 2022;17(1):47–51.
https://doi.org/10.5114/pg.2021.106083
Verras GI, Mulita F. Butyrylcholinesterase levels correlate with surgical site infection risk and severity after colorectal surgery: a prospective single-center study. Front Surg. 2024;11:1379410.
https://doi.org/10.3389/fsurg.2024.1379410
Bousis D, Verras GI, Bouchagier K, Antzoulas A, Panagiotopoulos I, Katinioti A, et al. The role of deep learning in diagnosing colorectal cancer. Prz Gastroenterol. 2023;18(3):266–273.
https://doi.org/10.5114/pg.2023.129494
Chlorogiannis DD, Verras GI, Tzelepi V, Chlorogiannis A, Apostolos A, Kotis K, et al. Tissue classification and diagnosis of colorectal cancer histopathology images using deep learning algorithms. Is the time ripe for clinical practice implementation? Prz Gastroenterol. 2023;18(4):353–367.
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2026 Peipei Shen, Tiantian Yang, Yawen Cong, Bin Zhang, Yu Xu, Benjie Xu, Shengjun Ji, Yutian Zhao, Yong Mao

This work is licensed under a Creative Commons Attribution 4.0 International License.









