Dose- and time-dependent effects of clodronate on orthodontic tooth movement
DOI:
https://doi.org/10.17305/bjbms.2017.1715Keywords:
Histology, tooth movement, pharmacology, bone biology, clodronate, bisphosphonateAbstract
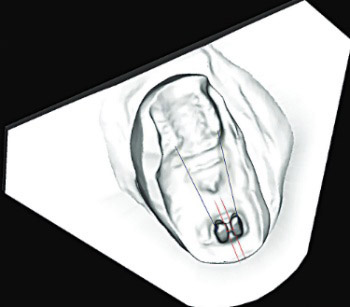
Orthodontic tooth movement is the result of bone remodeling that occurs in periodontal ligament and alveolar bone tissue as a response to mechanical loading of the tooth. The aim of this study is to investigate the time- and dose-response effects of locally administered clodronate on tooth movement. Sixty Wistar rats were randomly assigned to 4 groups of 15 specimens: E1 - application of 10 mMol of clodronate in 3-day intervals; E2 - application of 2.5 mMol of clodronate in 3-day intervals; E3 - application of 10 mMol of clodronate in 7-day intervals; E4 - application of 2.5 mMol of clodronate in 7-day intervals. A 50 μL clodronate solution was injected into a subperiosteal area to the right maxillary incisor. The left maxillary incisor served as a control, with an injection of saline solution. In 3-day interval application regime, there was no effect of clodronate dosing on tooth movement. In 7-day interval application regime, decreased tooth movement was observed with 10 mMol compared with 2.5 mMol clodronate concentration. However, decreased tooth movement was also observed when 2.5 mMol of clodronate was applied in 7-versus 3-day intervals. Conversely, no difference was observed when 10 mMol concentration was applied in 3- versus 7-day intervals. When clodronate is applied subperiosteally in the root area, it decreases the tooth movement. Tooth movement is impeded by the higher clodronate dosing, as well as by shorter application interval even with lower dosing. The purpose of future trials should, therefore, be to determine a safe therapeutic dose/interval application of clodronate in humans and their potential side effects.
Citations
Downloads
References
Garlet TP, Coelho U, Repeke CE, Silva JS, Cunha Fde Q, Garlet GP. Dif-ferential expression of osteoblast and osteoclast chemmoatractants in com-pression and tension sides during orthodontic movement. Cytokine 2008;42(3):330-5. https://doi.org/10.1016/j.cyto.2008.03.003.
Takano-Yamamoto T, Kawakami M, Kobayashi Y, Yamashiro T, Sakuda M. The effect of local application of 1,25-dihydroxycholecalciferol on os-teoclast numbers in orthodontically treated rats. J Dent Res 1992;71(1):53-9. https://doi.org/10.1177/00220345920710010901.
Mavragani M, Brudvik P, Selvig KA. Orthodontically induced root and alveolar bone resorption: Inhibitory effect of systemic doxycycline admin-istration in rats. Eur J Orthod 2005;27(3):215-25. https://doi.org/10.1093/ejo/cji015.
Baysal A, Uysal T, Ozdamar S, Kurt B, Kurt G, Gunhan O. Comparisons of the effects of systemic administration of L-thyroxine and doxycycline on orthodontically induced root resorption in rats. Eur J Orthod 2010;32(5):496-504. https://doi.org/10.1093/ejo/cjp124.
Russell RG. Bisphosphonates: The first 40 years. Bone 2011;49(1):2-19. https://doi.org/10.1016/j.bone.2011.04.022.
Igarashi K, Mitani H, Adachi H, Shinoda H. Anchorage and retentive ef-fects of a bisphosphonate (AHBuBP) on tooth movements in rats. Am J Orthod Dentofacial Orthop 1994;106(3):279-89. https://doi.org/10.1016/S0889-5406(94)70048-6.
Igarashi K, Adachi H, Mitani H, Shinoda H. Inhibitory effect of the topi-cal administration of a bisphosphonate (risedronate) on root resorption in-cident to orthodontic tooth movement in rats. J Dent Res 1996;75(9):1644-9. https://doi.org/10.1177/00220345960750090501.
Kim TW, Yoshida Y, Yokoya K, Sasaki T. An ultrastructural study of the effects of bisphosphonate administration on osteoclastic bone resorption during relapse of experimentally moved rat molars. Am J Orthod Dentofa-cial Orthop 1999;115(6):645-53.
https://doi.org/10.1016/S0889-5406(99)70290-8.
Rodrigues P, Hering F, Imperio M. Safety of I.V. nonnitrogen bisphos-phonates on the occurrence of osteonecrosis of the jaw: Long-term follow-up on prostate cancer patients. Clin Genitourin Cancer 2015;13(3):199-203. https://doi.org/10.1016/j.clgc.2014.10.001.
Frith JC, Mönkkönen J, Auriola S, Mönkkönen H, Rogers MJ. The mo-lecular mechanism of action of the antiresorptive and antiinflammatory drug clodronate: Evidence for the formation in vivo of a metabolite that inhibits bone resorption and causes osteoclast and macrophage apoptosis. Arthritis Rheum 2001;44(9):2201-10. https://doi.org/10.1002/1529-0131(200109)44:9<2201::AID-ART374>3.0.CO;2-E.
Liu L, Igarashi K, Haruyama N, Saeki S, Shinoda H, Mitani H. Effects of local administration of clodronate on orthodontic tooth movement and root resorption in rats. Eur J Orthod 2004;26(5):469-73. https://doi.org/10.1093/ejo/26.5.469.
Kilkenny C, Browne WJ, Cuthill IC, Emerson M, Altman DG. Improving bioscience research reporting: The ARRIVE guidelines for reporting animal research. PLoS Biol 2010;8(6):e1000412.
https://doi.org/10.1371/journal.pbio.1000412.
Arslan SG, Arslan H, Ketani A, Hamamci O. Effects of estrogen defi-ciency on tooth movement after force application: An experimental study in ovariectomized rats. Acta Odontol Scand 2007;65(6):319-23. https://doi.org/10.1080/00016350701678725.
Carvalho-Filho EP, Stabile AC, Ervolino E, Stuani MB, Iyomasa MM, Rocha MJ. Celecoxib treatment does not alter recruitment and activation of osteoclasts in the initial phase of experimental tooth movement. Eur J Hitochem 2012;56(4):e43. https://doi.org/10.4081/ejh.2012.e43.
Choi J, Baek SH, Lee JI, Chang YI. Effects of clodronate on early alveo-lar bone remodeling and root resorption related to orthodontic forces: A histomorphometric analysis. Am J Orthod Dentofacial Orthop 2010;138(5):548.e1-8. https://doi.org/10.1016/j.ajodo.2010.01.031.
Redlich M, Weinstock T, Abed Y, Schneor R, Holdstein Y, Fischer A. A new system for scanning, measuring and analyzing dental casts based on a 3D holographic sensor. Orthod Craniofac Res 2008;11(2):90-5. https://doi.org/10.1111/j.1601-6343.2007.00417.x.
Keating AP, Knox J, Bibb R, Zhurov AI. A comparison of plaster, digital and reconstructed study model accuracy. J Orthod 2008;35(3):191-201. https://doi.org/10.1179/146531207225022626.
Leifert MF, Leifert MM, Efstratiadis SS, Cangialosi TJ. Comparison of space analysis evaluations with digital models and plaster dental casts. Am J Orthod Dentofacial Orthop 2009;136(1):16.e1-4. DOI: 10.1016/j.ajodo.2008.11.019.
Fleisch H. New bisphosphonates in osteoporosis. Osteoporos Int 1993;3(S2):15-22. https://doi.org/10.1007/BF01623222.
Bagger YZ, Tankó LB, Alexandersen P, Ravn P, Christiansen C. Alen-dronate has a residual effect on bone mass in postmenopausal Danish women up to 7 years after treatment withdrawal. Bone 2003;33(3):301-7. https://doi.org/10.1016/S8756-3282(03)00112-1.
Rodan GA, Martin TJ. Therapeutic approaches to bone diseases. Science 2000;289(5484):1508-14. https://doi.org/10.1126/science.289.5484.1508.
Fleisch H. Development of bisphosphonates. Breast Cancer Res 2002;4(1):30-4. https://doi.org/10.1186/bcr414.
Sedghizadeh PP, Stanley K, Caligiuri M, Hofkes S, Lowry B, Shuler CF. Oral bisphosphonate use and the prevalence of osteonecrosis of the jaw: An institutional inquiry. J Am Dent Assoc 2009;140(1):61-6. https://doi.org/10.14219/jada.archive.2009.0019.
Mauri D, Valachis A, Polyzos IP, Polyzos NP, Kamposioras K, Pesce LL. Osteonecrosis of the jaw and use of bisphosphonates in adjuvant breast cancer treatment: A meta-analysis. Breast Cancer Res Treat 2009;116(3):433-9. https://doi.org/10.1007/s10549-009-0432-z.
Edwards BJ, Hellstein JW, Jacobsen PL, Kaltman S, Mariotti A, Migliorati CA, et al. Updated recommendations for managing the care of patients receiving oral bisphosphonate therapy: An advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 2008;139(12):1674-7. https://doi.org/10.14219/jada.archive.2008.0110.
Downloads
Additional Files
Published
How to Cite
Accepted 2016-11-22
Published 2017-02-21









