Anesthesia for patients with mucopolysaccharidoses: Comprehensive review of the literature with emphasis on airway management
DOI:
https://doi.org/10.17305/bjbms.2017.2201Keywords:
General anesthesia, lysosomal storage diseases, tracheal intubation, laryngoscopyAbstract
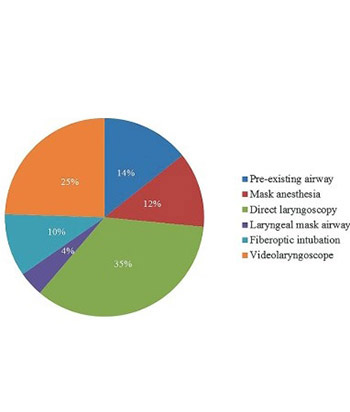
Mucopolysaccharidoses (MPS) are rare, inherited, lysosomal storage diseases that cause accumulation of glycosaminoglycans, resulting in anatomic abnormalities and organ dysfunction that can increase the risk of anesthesia complications. We conducted a systematic review of the literature in order to describe the anesthetic management and perioperative outcomes in patients with MPS. We reviewed English-language literature search using an OVID-based search strategy of the following databases: 1) PubMed (1946-present), 2) Medline (1946-present), 3) EMBASE (1946-present), and 4) Web of Science (1946-present), using the following search terms: mucopolysaccharidosis, Hurler, Scheie, Sanfilippo, Morquio, Maroteaux, anesthesia, perioperative, intubation, respiratory insufficiency, and airway. The review of the literature revealed nine case series and 27 case reports. A substantial number of patients have facial and oral abnormalities posing various challenges for airway management, however, evolving new technologies that include videolaryngoscopy appears to substantially facilitate airway management in these patients. The only type of MPS that appears to have less difficulty with airway management are MPS III patients, as the primary site of glycosaminoglycan deposition is in the central nervous system. All other MPS types have facial and oral characteristics that increase the risk of airway management. To mitigate these risks, anesthesia should be conducted by experienced anesthesiologists with expertise in using of advanced airway intubating devices.
Citations
Downloads
References
Muenzer J. Overview of the mucopolysaccharidoses. Rheumatology (Oxford) 2011;50(Suppl 5):v4-12. https://doi.org/10.1093/rheumatology/ker394.
Baines D. Suxamethonium in mucopolysaccharidosis. Anaesth Intensive Care 1989;17(3):382.
Kempthorne PM, Brown TC. Anaesthesia and the mucopolysaccharidoses: A survey of techniques and problems. Anaesth Intensive Care 1983;11(3):203-7.
King DH, Jones RM, Barnett MB. Anaesthetic considerations in the mucopolysaccharidoses. Anaesthesia 1984;39(2):126-31. https://doi.org/10.1111/j.1365-2044.1984.tb09499.x.
Walker R, Belani KG, Braunlin EA, Bruce IA, Hack H, Harmatz PR, et al. Anaesthesia and airway management in mucopolysaccharidosis. J Inherit Metab Dis 2013;36(2):211-9. https://doi.org/10.1007/s10545-012-9563-1.
Arn P, Wraith JE, Underhill L. Characterization of surgical procedures in patients with mucopolysaccharidosis Type I: Findings from the MPS I Registry. J Pediatr 2009;154(6):859-64.e3. https://doi.org/10.1016/j.jpeds.2008.12.024.
Mendelsohn NJ, Harmatz P, Bodamer O, Burton BK, Giugliani R, Jones SA, et al. Importance of surgical history in diagnosing mucopolysaccharidosis Type II (Hunter syndrome): Data from the hunter outcome survey. Genet Med 2010;12(12):816-22. https://doi.org/10.1111/j.1460-9592.2012.03825.x.
Frawley G, Fuenzalida D, Donath S, Yaplito-Lee J, Peters H. A retrospective audit of anesthetic techniques and complications in children with mucopolysaccharidoses. Paediatr Anaesth 2012;22(8):737-44. https://doi.org/10.1111/j.1460-9592.2012.03825.x.
Megens JH, de Wit M, van Hasselt PM, Boelens JJ, van der Werff DB, de Graaff JC. Perioperative complications in patients diagnosed with mucopolysaccharidosis and the impact of enzyme replacement therapy followed by hematopoietic stem cell transplantation at early age. Paediatr Anaesth 2014;24(5):521-7. https://doi.org/10.1111/pan.12370.
Moores C, Rogers JG, McKenzie IM, Brown TC. Anaesthesia for children with mucopolysaccharidoses. Anaesth Intensive Care 1996;24(4):459-63.
Cohen-Levy J. Orthodontic treatments of pediatric obstructive sleep apnea syndrome. Med Sommeil 2011;8(2):61-8. https://doi.org/10.1016/j.msom.2011.03.001.
Cohen MA, Stuart GM. Delivery of anesthesia for children with Mucopolysaccharidosis Type III (Sanfilippo syndrome): A review of 86 anesthetics. Paediatr Anaesth 2017;27(4):363-9. https://doi.org/10.1111/pan.13075.
Kamata M, McKee C, Truxal KV, Flanigan KM, McBride KL, Aylward SC, et al. General anesthesia with a native airway for patients with mucopolysaccharidosis Type III. Paediatr Anaesth 2017;27(4):370-6. https://doi.org/10.1111/pan.13108.
Cingi EC, Beebe DS, Whitley CB, Belani KG. Anesthetic care and perioperative complications in children with Sanfilipo Syndrome Type A. Paediatr Anaesth 2016;26(5):531-8. https://doi.org/10.1111/pan.12876.
Clark BM, Sprung JJ, Weingarten TN, Warner ME. Airway management changes in patients with mucopolysaccharidoses: The role of videolaryngoscopy. Can J Anaesth 2017 [Epub ahead of print]. https://doi.org/10.1007/s12630-017-0906-0.
Cade J, Jansen N. Anesthetic challenges in an adult with mucopolysaccharidosis Type VI. A&A Case Rep 2014;2(12):152-4. https://doi.org/10.1213/XAA.0000000000000031.
Gurumurthy T, Shailaja S, Kishan S, Stephen M. Management of an anticipated difficult airway in Hurler's syndrome. J Anaesthesiol Clin Pharmacol 2014;30(4):558-61. https://doi.org/10.4103/0970-9185.142862.
Ziyaeifard M, Azarfarin R, Ferasatkish R, Dashti M. Management of difficult airway with laryngeal mask in a child with mucopolysaccharidosis and mitral regurgitation: A case report. Res Cardiovasc Med 2014;3(2):e17456. https://doi.org/10.5812/cardiovascmed.17456.
Nadeem A, Siddiqui K. Anaesthesia challenges in a patient with Hurler syndrome: A case report. Anaesth Pain Intensive Care 2012;16(1):100-1.
Gupta N, Rath GP, Bala R, Reddy BK, Chaturvedi A. Anesthetic management in children with Hurler's syndrome undergoing emergency ventriculoperitoneal shunt surgery. Saudi J Anaesth 2012;6(2):178-80. https://doi.org/10.4103/1658-354X.97036.
Ard JL Jr, Bekker A, Frempong-Boadu AK. Anesthesia for an adult with mucopolysaccharidosis I. J Clin Anesth 2005;17(8):624-6. https://doi.org/10.1016/j.jclinane.2005.01.012.
Walker RW, Dearlove OR. Anaesthesia for children with mucopolysaccharidoses. Anaesth Intensive Care 1997;25(2):197-8.
Wilder RT, Belani KG. Fiberoptic intubation complicated by pulmonary edema in a 12-year-old child with Hurler syndrome. Anesthesiology 1990;72(1):205-7. https://doi.org/10.1097/00000542-199001000-00033.
Busoni P, Fognani G. Failure of the laryngeal mask to secure the airway in a patient with Hunter's syndrome (mucopolysaccharidosis Type II). Paediatr Anaesth 1999;9(2):153-5. https://doi.org/10.1046/j.1460-9592.1999.9220289.x.
Kaur J, Swami AC, Kumar A, Lata S. Anesthetic management of a child with Hunter's syndrome. J Anaesthesiol Clin Pharmacol 2012;28(2):255-7.
https://doi.org/10.4103/0970-9185.94914.
Dhanger S, Adinarayanan S, Vinayagam S, Kumar MP. I-gel assisted fiberoptic intubation in a child with Morquio's syndrome. Saudi J Anaesth 2015;9(2):217-9. https://doi.org/10.4103/1658-354X.152893.
Morgan KA, Rehman MA, Schwartz RE. Morquio's syndrome and its anaesthetic considerations. Paediatr Anaesth 2002;12(7):641-4.
https://doi.org/10.1046/j.1460-9592.2002.00838.x.
Bartz HJ, Wiesner L, Wappler F. Anaesthetic management of patients with mucopolysaccharidosis IV presenting for major orthopaedic surgery. Acta Anaesthesiol Scand 1999;43(6):679-83. https://doi.org/10.1034/j.1399-6576.1999.430614.x.
Nielsen RM, Pedersen NA, Olsen KS. Airway management in a patient with Morquio-Brailsford syndrome. Eur J Anaesthesiol 2013;30(3):133-4. https://doi.org/10.1097/EJA.0b013e32835c8dc5.
Chaudhuri S, Duggappa AK, Mathew S, Venkatesh S. Safe intubation in Morquio-Brailsford syndrome: A challenge for the anesthesiologist. J Anaesthesiol Clin Pharmacol 2013;29(2):258-61. https://doi.org/10.4103/0970-9185.111666.
Kadic L, Driessen JJ. General anaesthesia in an adult patient with Morquio syndrom with emphasis on airway issues. Bosn J Basic Med Sci 2012;12(2):130-3.
Shivajirao TP, Wasmatkar NP, Gore PG, Lakhe JN, Vinayak SR. Anesthetic considerations in Morquio syndrome: A case report. Anaest Pain Intensive Care 2013;17(1):75-8.
McLaughlin AM, Farooq M, Donnelly MB, Foley K. Anaesthetic considerations of adults with Morquio's syndrome - A case report. BMC Anesthesiol 20106;10:2.
Pagel PS, Almassi GH. Perioperative implications of Morquio syndrome in a 31-year-old woman undergoing aortic valve replacement. J Cardiothorac Vasc Anesth 2009;23(6):855-7. https://doi.org/10.1053/j.jvca.2008.12.009.
Sayilgan C, Yuceyar L, Akbas S, Erolcay H. Anesthesia in a child with Maroteaux-Lamy syndrome undergoing mitral valve replacement. Clinics (Sao Paulo) 2012;67(6):693-6. https://doi.org/10.6061/clinics/2012(06)26.
Suh SH, Okutani R, Nakasuji M, Nakata K. Anesthesia in a patient with mucopolysaccharidosis Type VI (Maroteaux-Lamy syndrome). J Anesth 2010;24(6):945-8. https://doi.org/10.1007/s00540-010-1029-8.
Barbosa FT, Borges EL, Brandão RR. General anesthesia after failed spinal block for emergency surgery in a patient with mucopolysaccharidosis: Case report. [Article in Portuguese]. Rev Bras Anestesiol 2007;57(6):658-64.
Arn P, Whitley C, Wraith JE, Webb HW, Underhill L, Rangachari L, et al. High rate of postoperative mortality in patients with mucopolysaccharidosis I: Findings from the MPS I Registry. J Pediatr Surg 2012;47(3):477-84. https://doi.org/10.1016/j.jpedsurg.2011.09.042.
Kumar KR, Kumar H, Baidya DK, Arora MK. Successful use of spinal anesthesia for inguinal hernia repair in a child with Hunter syndrome with difficult airway. J Clin Anesth 2016;30:99-100. https://doi.org/10.1016/j.jclinane.2015.08.025.
Theroux MC, Nerker T, Ditro C, Mackenzie WG. Anesthetic care and perioperative complications of children with Morquio syndrome. Paediatr Anaesth 2012;22(9):901-7. https://doi.org/10.1111/j.1460-9592.2012.03904.x.
Tomatsu S, Averill LW, Sawamoto K, Mackenzie WG, Bober MB, Pizarro C, et al. Obstructive airway in Morquio A syndrome, the past, the present and the future. Mol Genet Metab 2016;117(2):150-6. https://doi.org/10.1016/j.ymgme.2015.09.007.
Cingi E, Belani K, Beebe D, Apostolidou I, Whitley C. Anesthetic care and outcome in children with Sanfilippo syndrome type A. Mol Gen Metab 2013;108(2):S30. http://dx.doi.org/10.1016/j.ymgme.2012.11.056.
Osthaus WA, Harendza T, Witt LH, Jüttner B, Dieck T, Grigull L, et al. Paediatric airway management in mucopolysaccharidosis 1: A retrospective case review. Eur J Anaesthesiol 2012;29(4):204-7. https://doi.org/10.1097/EJA.0b013e328350677b.
Walker PP, Rose E, Williams JG. Upper airways abnormalities and tracheal problems in Morquio's disease. Thorax 2003;58(5):458-9. https://doi.org/10.1136/thorax.58.5.458.
Hack HA, Walker R, Gardiner P. Anaesthetic implications of the changing management of patients with mucopolysaccharidosis. Anaesth Intensive Care 2016;44(6):660-8.
Walker RW, Allen DL, Rothera MR. A fibreoptic intubation technique for children with mucopolysaccharidoses using the laryngeal mask airway. Paediatr Anaesth 1997;7(5):421-6. https://doi.org/10.1046/j.1460-9592.1997.d01-102.x.
Downloads
Additional Files
Published
How to Cite
Accepted 2017-06-01
Published 2018-02-20









