An assessment of correlation between serum asymmetric dimethylarginine and glycated haemoglobin in patients with type 2 diabetes mellitus
DOI:
https://doi.org/10.17305/bjbms.2014.2291Keywords:
asymmetric dimethylarginine, endothelial dysfunction, glycated haemoglobin, type 2 diabetes mellitusAbstract
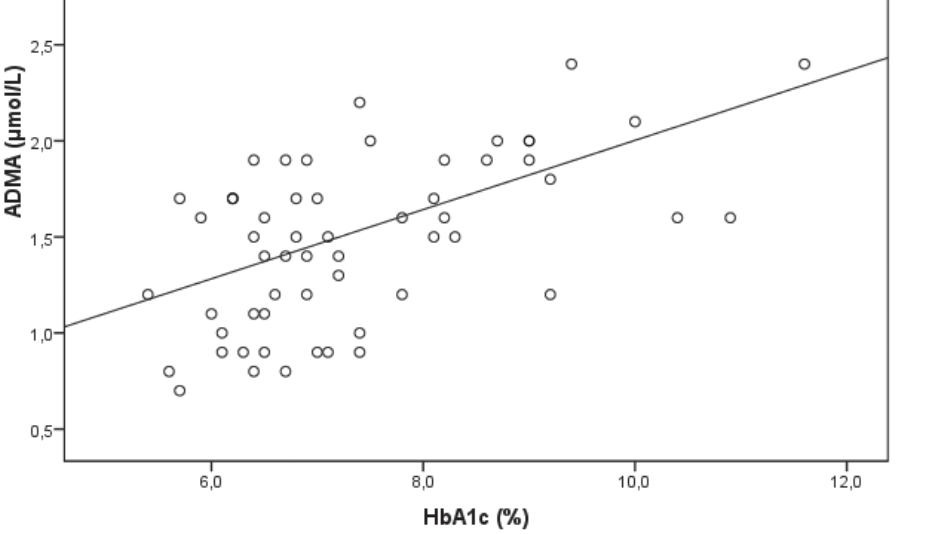
Studies that investigated an association between asymmetric dimethylarginine (ADMA) and glycated haemoglobin (HbA1c) in type 2 diabetes mellitus (T2DM) have given discordant results. The aim of this study was to determine and compare serum ADMA concentration in patients with T2DM and healthy controls, and to assess correlation between ADMA and HbA1c in patients with T2DM. Serum ADMA concentration was determined by ELISA method with the use of ADMA ® - ELISA kit (DLD Diagnostics, Hamburg, Germany) and HbA1c levels were determined by an immunoturbidimetric method in 60 patients with T2DM and 60 healthy individuals matched for age and sex. Results have shown that mean serum ADMA concentration was significantly higher in T2DM patients (1.54±0.06 μmol/L) compared to mean serum ADMA concentration (0.62±0.02 μmol/L; p<0.0001) in healthy subjects. A significant, positive, correlation between serum ADMA concentration and HbA1c levels was observed (r=0.494; p<0.01) in T2DM patients. Our results suggest that there is an association between endothelial dysfunction and glycaemic control in type 2 diabetes mellitus. Possible explanation for obtained results may be oxidative stress that is increased in conditions of hyperglycaemia and it also promotes endothelial dysfunction. Larger, longitudinal studies are required that will evaluate relation between metabolic abnormalities and increased ADMA levels in patients with type 2 diabetes mellitus.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2017 Bosnian Journal of Basic Medical Sciences

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2017-07-19
Published 2014-05-20









