A histological study of the effect of exogenous melatonin on gentamicin induced structural alterations of proximal tubules in rats
DOI:
https://doi.org/10.17305/bjbms.2014.2293Keywords:
gentamicin, melatonin, proximal tubules, rats, histological analysisAbstract
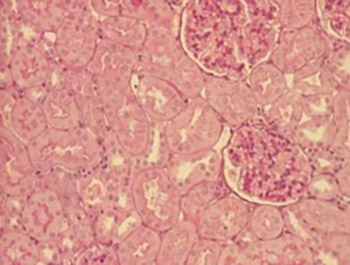
The aim of this research was to assess the reactive changes of rat proximal tubules caused by gentamicin and the effect of relatively low doses of melatonin. 48 adult male Wistar rats were distributed into six groups of equal size which all received one of the following daily intraperitoneal injections: vehicle (5% ethanol in Ringer solution) during 11 days (C); gentamicin (80 mg/kg) during 8 days (G), two groups which concomitantly received gentamicin (80 mg/kg) during 8 days and melatonin in two different test doses (5 or 20 mg/kg) during 11 days (GM1, GM2) and two groups treated only with melatonin in two different doses (5 or 20 mg/kg) during 11 days (M1, M2). Histological analysis included qualitative and semi-quantitative light microscopy analysis of proximal tubules. Exogenous melatonin had no significant effect on the microstructure, independently of dosis. The changes of proximal tubules microstructure induced by gentamicin were expressed in the form of granulovacuolar degeneration, necrosis and desquamation. The grade of proximal tubular changes was smaller in animals who besides gentamicin received melatonin. Melatonin has a dose dependent protective effect on the structural alterations of proximal tubules of the kidney induced by gentamicin.
Citations
Downloads
Downloads
Additional Files
Published
How to Cite
Accepted 2017-07-19
Published 2014-05-20









