Solitary intracranial tuberculoma mimicking a malignant tumor in a patient without tubercular lesions or a history of disease: a case report
DOI:
https://doi.org/10.17305/bjbms.2013.2396Keywords:
tuberculosis, intracranial tuberculoma, tomography x-ray computed, magnetic resonance imaging, polymerase chain reactionAbstract
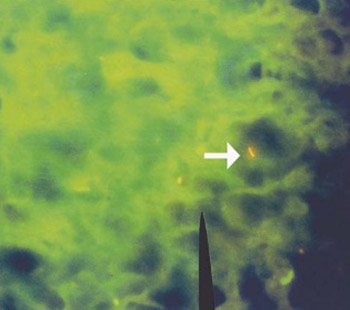
Cerebral tuberculoma is a rare cause of intracranial mass. In Latin America and Colombia where tuberculosis is endemic, it represents between 5 and 30% of brain tumours. A 53-year-old Colombian woman was admitted to a third-level hospital in Cali, Colombia, after reporting loss of consciousness, headache, paresthesia, and flight of ideas for a two-week period. Imaging studies showed a left frontal mass of malignant appearance whose first possible diagnosis was metastatic neoplasia or glioma. With the initial results, absence of history of chronic infectious diseases and a history of thyroidectomy, a surgical procedure was carried out and a histopathological and molecular evaluation was conducted. The pathology report noted necrotizing granulomatous inflammation and tissue staining and molecular tests for detection of M. tuberculosis were positive and the patient was managed with anti-tubercular treatment. Intracranial masses are frequently targeted as a malignant neoplastic disease for surgical treatment. Considering an infectious etiology must be a diagnostic option.
Citations
Downloads
Downloads
Additional Files
Published
How to Cite
Accepted 2017-08-30
Published 2013-05-20









