A comparison of the in vitro cytotoxicity of conventional and resin modified glass ionomer cements
DOI:
https://doi.org/10.17305/bjbms.2012.2454Keywords:
conventional and resin-modified glass-ionomer cements, cytotoxicity tests, colorimetric assayAbstract
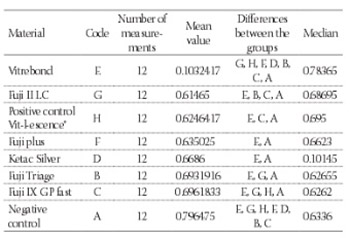
To evaluate cytotoxicity of experimental conventional and resin modified glass-ionomer cements on UMR-106 osteoblast cell cultures and cell cultures of NIH3T3 mouse fibroblasts specimens were prepared for every experimental material and divided into: group 1. Conventional glass-ionomer cements: GC Fuji IX GP Fast, GC Fuji Triage and Ketac Silver; group 2. Resin modified glass-ionomer cements: GC Fuji II LC, GC Fuji Plus and Vitrebond; group 3. Positive control was presented by specimens of composite Vit-l-ecence® and negative control-group 4. was presented by α-minimum essential medium for UMR-106 – osteoblast-like cells and Dulbecco’s Modified Eagle’s Medium for NIH3T3 mouse fibroblast cells. Both cell cultures were exposed to 10% of eluate of each single specimen of each experimental material. Experimental dishes were incubated for 24 h. Cell metabolism was evaluated using methyltetrazolium assay. Kruskal-Wallis test and Tukey-Kramer post hoc test for the materials evaluated on NIH3T3 mouse fibroblast cells, as well as UMR-106 osteoblast-like cells showed significantly more cytotoxicity of RMGICs, predominantly Vitrebond to both GICs and composite-Vit-l-ecence®. The lowest influence on cell’s metabolism on UMR-106 osteoblas-like cells was shown by Ketac Silver and the lowest influence on cell’s metabolism on NIH3T3 mouse fibroblast cells was shown by Fuji IX GP Fast. Statistical evaluation of sensitivity of cell lines UMR-106 osteoblast-like cells and NIH3T3 mouse fibroblast cells, using Mann-Whitney test, showed that NIH3T3 mouse fibroblast cells were more sensitive for the evaluation of cytotoxicity of dental materials.
Citations
Downloads
Downloads
Additional Files
Published
How to Cite
Accepted 2017-09-14
Published 2012-11-20









