Bladder outlet obstruction number- a good indicator of infravesical obstruction in patients with benign prostatic enlargement?
DOI:
https://doi.org/10.17305/bjbms.2012.2459Keywords:
benign prostatic enlargement, bladder outlet obstruction number, urodynamicsAbstract
The objective of our study was to evaluate bladder outlet obstruction number (BOON) in order to predict infravesical obstruction in patients with benign prostatic enlargement (BPE).
Two hundred patients with proven BPE from daily urological practice at the Urology Department of the Sarajevo University Clinical Centre were covered by a prospective study in period 2009-2011. All patients completed International Prostatic Symptom Score, their mean voided volume urine was determined from frequency-volume chart and their prostate volume was determined by transabdominal ultrasound. Subsequently, the patients had free uroflowmetry and they underwent complete urodynamic studies.
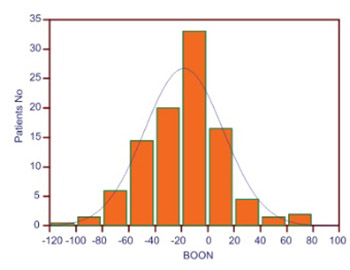
BOON was calculated using the formula: prostate volume (cc)-3 x Qmax (ml/s)-0.2 x mean voided volume (ml). A satisfactory area under the curve (AUC) was obtained for the prediction of obstruction according to bladder outlet obstruction index, Schaefer obstruction class nomogram and group specific urethral resistance factor, with AUC of 0.83 (p<0.001). Following the comparison of different cut-off values of BOON according to the obstruction, the BOON >-20 has been found to be the most accurate obstruction indicator (sensitivity 76.5% and specificity 68.2%), with posttest probability of 77%.
The BOON may be used in daily urological practice as a valid, non-invasive indicator of infravesical obstruction in patients with BPE, with a possibility of correct classification of obstruction in approximately 75% of the cases. Transabdominal ultrasound has shown to be applicable to the BOON formula in determining prostate volume.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2017-09-15
Published 2012-08-20









