Brain natriuretic peptide release in acute myocardial infarction
DOI:
https://doi.org/10.17305/bjbms.2012.2470Keywords:
brain natriuretic peptide, acute myocardial infarction, left ventricle systolic dysfunctionAbstract
Brain natriuretic peptide (BNP) is released from ventricular myocites due to their stretching and volume overload. In heart failure there is BNP release. Aim of this study was to observe BNP release in acute myocardial infarction (AMI).
We measured BNP in 75 patients with AMI. Control group (n=61) was similar by age and gender to AMI group.
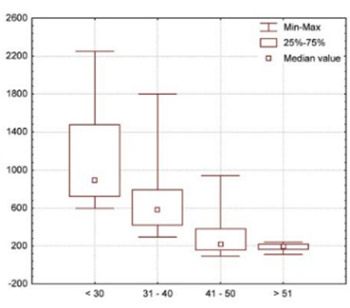
We found statistically significant elevation of BNP compared to controls (462.875 pg/ml vs 35.356 pg/ml,p< 0.001). Patients with severe systolic dysfunction had the highest BNP levels, while patients with the preserved systolic function had the lowest BNP levels (Group with EF<30% BNP= 1129.036 pg/ml vs Group with EF31-40 % BNP= 690.177 pg/ml vs Group with EF 41-50% BNP= 274.396 pg/ml vs Group with EF>51% BNP= 189.566 pg/ml, p< 0.001). We found statistically significant light positive correlation between BNP and left ventricle end-diastolic diameter (LVDd) (r= 0.246,p<0.05). and real positive correlation between BNP and peak troponin levels (r= 0.441,p < 0.05). BNP levels were higher in anteroseptal allocation of AMI compared to inferior allocation (835.80 pg/ml vs 243.03 pg/ml, p< 0.001) and in patients who were treated with heparin compared to fibrinolitic therapy (507.885 pg/ml vs 354.73 pg/ml, p< 0.05).
BNP is elevated in AMI and is a quantitative biochemical marker related to the extent of infarction and the left ventricle systolic dysfunction. Besides echocardiographic calculation, elevation of BNP could be used for quick and easy determination of the left ventricle systolic dysfunction.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2017-09-20
Published 2012-08-20









