Persistent submacular fluid diagnosed with Optical Coherence Tomography after successful scleral buckle surgery for macula-off retinal detachment
DOI:
https://doi.org/10.17305/bjbms.2012.2479Keywords:
macula-off retinal detachment, scleral buckle surgery, optical coherence tomography, submacular fluidAbstract
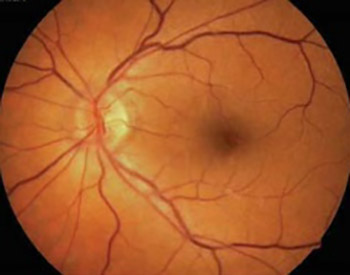
The objective of our study was to analyze the presence of persistent submacular fluid after apparently successful scleral buckle surgery for macula-off retinal detachment, using Optical Coherence Tomography (OCT), and to correlate these findings to postoperative visual acuity. Prospective study of consecutive patients hospitalized for macula-off retinal detachment, between February 2008 and April 2010, was carried out at the single referral centre for vitreoretinal surgery in Serbia. Outcomes were evaluated 1, 3, 6 and 12 months postoperatively, using OCT and best corrected visual acuity (BCVA). All 48 patients with macula-off retinal detachment had undergone clinically successful scleral buckle surgery, 3 to 30 days (mean 14.2 ± 6.9) after the onset of symptoms. Reattachment was achieved and one month later, patients were divided in two groups, according to the presence of submacular fluid assessed by OCT group A with detectable residual submacular fluid (40%) and group B without (60%).
The mean BCVA one month postoperatively was significantly lower (p<0.01) in the group A (0.11 ± 0.03) opposed to the group B (0.51 ± 0.11).
However, after a 12-month-follow-up, BCVA was similar in both groups (0.52 ± 0.17 and 0.54 ± 0.15 respectively, p=0.541), due to the restitution of normal macular architecture confirmed by OCT.
The prolonged recovery of visual acuity in patients with macula-off retinal detachment who had undergone successful scleral buckle surgery could be explained with presence of submacular fluid, diagnosed by OCT. However, final visual outcome was favourable, due to the gradual resorption of submacular fluid in a 12-month-period.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2017-09-21
Published 2012-08-20









