TREM-1 is a positive regulator of TNF-α and IL-8 production in U937 foam cells
DOI:
https://doi.org/10.17305/bjbms.2012.2503Keywords:
TREM-1, foam cell, TNF-α, IL-8, atherosclerosisAbstract
The purpose of our study was to investigate the expression levels of TREM-1 (triggering receptor expressed on myeloid cells-1) in U937 foam cells and determine whether TREM-1 regulates the production of tumor necrosis factor-alpha and interleukin-8 in these cells.
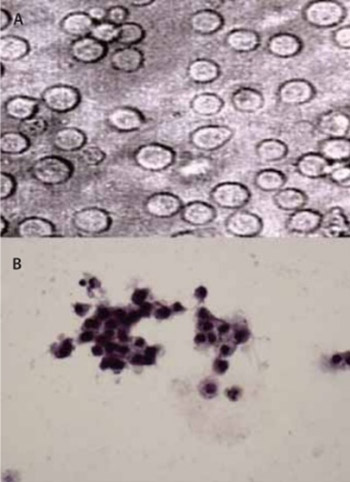
Human U937 cells were incubated with phorbol 12-myristate 13-acetate and then oxidized human low-density lipoprotein to induce foam cell formation. Oil red O staining was used to identify the foam cells. The production of IL-8 and TNF-α by U937 foam cells was assayed by enzyme-linked immunosorbent assay. The expression of TREM-1 mRNA in U937 foam cells was detected by reverse transcription-polymerase chain reaction. Moreover, U937 foam cells were transfected by small interfering RNA using Lipofectamine 2000 to knockdown TREM-1. Western blot was performed to assay protein expression of TREM-1 and ELISA was used to examine the effect of TREM-1 knockdown on IL-8 and TNF-α production.
PMA and ox-LDL induced U937 cells to form foam cells. The production of TNF-α and IL-8 was found to be significantly elevated in U937 foam cells, concomitant with a significant up-regulation of TREM-1 mRNA. TREM-1 siRNA was able to partially silence the expression of TREM-1 protein and remarkably inhibited TNF-α and IL-8 production in U937 foam cells, suggesting that TREM-1 is a positive regulator of TNF-α and IL-8 production in U937 foam cells.
Our finding that TREM-1 controls the production of IL-8 and TNF-α in U937 foam cells defines a potentially critical role of TREM-1 in the pathogenesis of atherosclerosis and implicates TREM-1 as a potential therapeutic target for the disease.
Citations
Downloads
Downloads
Additional Files
Published
How to Cite
Accepted 2017-09-26
Published 2012-05-20









