The effect of continuous jejunal interposition on gastrointestinal hormones after distal gastrectomy
DOI:
https://doi.org/10.17305/bjbms.2012.2524Keywords:
distal gastrectomy, continuous jejunal interpositionon, serum gastrin plasma motilin, sholecystokininAbstract
The objective of our study was to determine the effect of continuous jejunal interposition on gastrointestinal hormones after distal gastrectomy, and lay a foundation for surgical management.
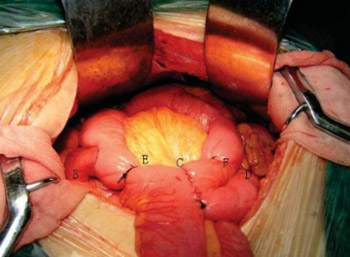
Distal subtotal gastrectomy experimental model were established on 24 adult Beagle dogs. Digestive tract reconstruction of the dogs was randomly divided into continuous jejunal interposition group, Billroth II anastomosis group and isolated jejunum interposition group. The content of serum gastrin, plasma motilin and cholecystokinin after different digestive tract reconstructions was detected and compared by enzyme-linked immunosorbent assay
In the dogs which received continuous jejunal interposition, postoperative serum gastrin level was significantly lower than before surgery either in fasting or postprandial state (all p<0.05). The serum gastrin level of continuous jejunal interposition group was significantly higher than the other groups in postprandial state (all p<0.05), and was significantly higher than Billroth II -type anastomosis group in fasting state (p<0.05). Furthermore, the postoperative plasma motilin and cholecystokinin levels were significantly higher than before surgery either in fasting or postprandial in dogs received continuous jejunal interposition (all p<0.05). The postoperative plasma motilin level of continuous jejunal interposition group was significantly higher than the other groups in postprandial state (all p<0.05), and was significantly higher than Billroth II -type anastomosis group in fasting state (p<0.05). However, the postoperative cholecystokinin level of continuous jejunal interposition group was significantly lower than the other groups (allp p<0.05).
Continuous jejunal interposition after distal gastrectomy could maintain the postoperative plasma motilin and serum gastrin in a relatively high level, while cholecystokinin in a low level.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2017-10-02
Published 2012-02-20









