High grade intraepithelial neoplasia of prostate is associated with values of prostate specific antigen related parameters intermediate between prostate cancer and normal levels
DOI:
https://doi.org/10.17305/bjbms.2011.2551Keywords:
prostate intraepithelial neoplasia, prostate specific antigenAbstract
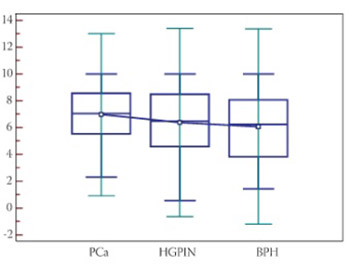
High grade prostatic intraepithelial neoplasia (HGPIN) is widely regarded as the precancerous. The aim of this study was to determine PSA related parameters in patients with initial PSA values 2-10 ng/mL and diagnosis of HGPIN without finding carcinoma at the time of their first needle biopsy. Study groups consisted of 100 men who were diagnosed HGPIN, 84 with cancer and 183 with benign hyperplasia on first biopsy of prostate. Total PSA and free PSA were measured and ratio free/total PSA and PSA density calculated. Mean values of these parameters were compared, and receiver operating characteristic curves were used for comparison of PSA related parameters to discriminate groups of patients. Total PSA, free PSA level and PSA density in patients with HGPIN (6.388 ng/mL) did not differ significantly compared to prostate carcinoma (6.976 ng/mL) or benign prostatic hyperplasia (6.07 ng/mL) patients. Patients with HGPIN had significantly higher ratio free/total PSA than those with prostate carcinoma (0.168 vs 0.133), but significantly lower than patients with benign prostatic hyperplasia (0.168 vs 0.185). Ratio of free/total PSA significantly discriminate HGPIN from prostate carcinoma with sensitivity 84.52 and specify 45.00 at cut-off point of ≤ 0.18. Values of PSA, free PSA and ratio free/total PSA in cases of HGPIN appear to be intermediate between prostate cancer and normal levels. Ratio of free/total PSA may help in decision to repeat biopsies in the presence of HGPIN on biopsy, without concomitant prostate cancer, in patients suitable for curative treatment, with normal digito-rectal examination and trans-rectal sonography.
Citations
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2017-10-11
Published 2011-11-20









