Endothelial dysfunction in uremic patients on continuous ambulatory peritoneal dialysis (CAPD)
DOI:
https://doi.org/10.17305/bjbms.2011.2566Keywords:
CAPD patients, endothelial dysfunctionAbstract
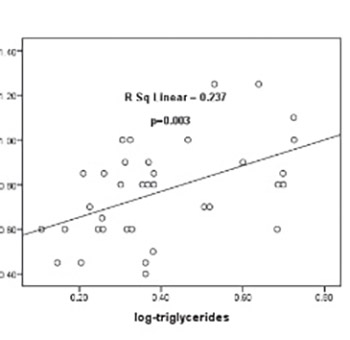
Endothelial dysfunction is associated with diabetic micro- and macroangiopathy as well as with the decline in creatinine clearance. It has been suggested that endothelial dysfunction presents in patients (pts) on continuous ambulatory peritoneal dialysis (CAPD). The objective of this study was to examine the plasma biomarkers of endothelial dysfunction and their association with IMT of carotid arteries in diabetic and non-diabetic patients on CAPD. This study included 37 CAPD pts (25 with type II diabetes and 12 non-diabetic pts) mean age 59.2 years ± 2.48. Plasma von Willebrand factor (vWF) activity, serum albumin, glucose, total cholesterol, triglycerides and lipoprotein (a) levels, as well as serum level of homocysteine, parathyroid hormone (PTH) in plasma and microalbuminuria was determined. Ultrasound examination of carotid arteries was performed in all patients by measured bilateral intima-media thickness of carotid artery (CIMT). Mean IMT value was significantly higher in type 2 DM patients (0.86 ± 0.04 mm) compared to non-diabetic patients (0.52 ± 0.06 mm) on peritoneal dialysis (p<0.0001). There was also a significant difference in lipids/triglycerides and Lp (a)/, procoagulation (fibrinogen, von Wilebrand factor, factor VIII) and inflammatory markers (CRP) level between type 2 DM and non-diabetic CAPD patients. A stepwise multiple regression analysis revealed that log triglycerides and factor VIII were independent factors for the IMT. The results of this research impose that diabetic type 2 CAPD patients have developed systemic alteration of endothelial function and higher risk of cardiovascular complications compared to non-diabetic CAPD patients.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2017-10-15
Published 2011-08-20









