Lung 99mTc-MIBI scintigraphy: impact on diagnosis of solitary pulmonary nodule
DOI:
https://doi.org/10.17305/bjbms.2011.2570Keywords:
99mTc-Sestamibi, radionuclide imaging, solitary pulmonary nodule, diagnosisAbstract
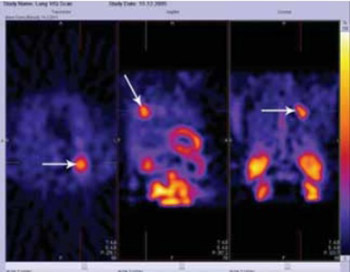
Most of today available non-invasive procedures cannot clearly determinate between benign and malignant solitary pulmonary nodules (SPN). The purpose of the study was to assess the possibility of using 99mTc labeled hexakis-2-methoxyisobutylisonitrile (99mTc-MIBI) to differentiate benign from malignant SPN. Sixty patients were included in the study if the CT scan showed indeterminate SPN. Prior to definitive diagnosis 99mTc-MIBI single photon emission computerized tomography (SPECT) was performed: early scan 10 minutes and delayed 60-120 minutes after the intravenous injection of 740 MBq 99mTc-MIBI using dual-headed Gamma camera. The results were considered positive if there was an increased accumulation of the radiopharmaceutical in the area of the lung corresponding to the location of the lesion.
The mean nodule size ± SD measured on CT scan was 2.96 cm. Lung cancer was diagnosed in 30/60 patients (14 squamocellular, 10 adenocarcinoma, 3 large-cell and 3 microcellular lung carcinomas). Of the 30 patients with malignant lesions, 27 patients (90%) had positive 99mTc-MIBI scan results by qualitative assessment. Among benign lesions, 23/30 (76.7%) were negative on 99mTc-MIBI scan. The size and PH report of SPN is statistically significantly influencing on 99mTc-MIBI accumulation in the SPN (p<0.01). The sensitivity, specificity, accuracy, positive and negative predictive value were 90%, 76.6%, 79.4%, 88.5% and 83.3% respectively.
99mTc-MIBI SPECT is an inexpensive non-invasive diagnostic procedure which might be useful diagnostic modality in the evaluation of SPN. Easy availability and low cost makes 99mTc-MIBI SPECT an attractive method in evaluating SPN.
Citations
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2017-10-16
Published 2011-08-20









