Collet Sicard syndrome as atypical presentation of neck fibrosarcoma: a case report
DOI:
https://doi.org/10.17305/bjbms.2011.2600Keywords:
fibrosarcoma, neck, Collet Sicard syndromeAbstract
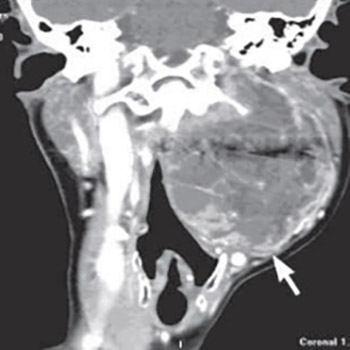
We report a 57 years old female patient with neck fibrosarcoma. Her main complaints consisted of hoarseness, difficulty swallowing, pain in the left side of her neck and left shoulder region, which all indicated the Collet Sicard syndrome, so the working diagnosis was glomus tumor Diagnostic MSCT was used, and the characteristics of the radiologic finding did not indicate any of the paraganglioma types, although the tumor was localized in the area of the carotid bifurcation, demonstrating the signs of extension into the jugular foramen. The patient has been treated surgically in general anesthesia and pathologic diagnosis was fibrosarcoma.
Citations
Downloads
Additional Files
Published
How to Cite
Accepted 2017-10-23
Published 2011-05-20









