Vascular patterns of upper limb: an anatomical study with accent on superficial brachial artery
DOI:
https://doi.org/10.17305/bjbms.2011.2615Keywords:
anatomical variations, axillary artery, profunda brachii artery, superficial brachial arteryAbstract
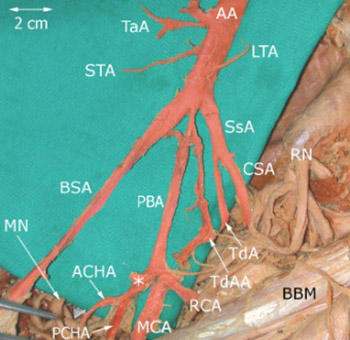
The aim of the study was to evaluate the terminal segmentation of the axillary artery and to present four cases of anomalous branching of the axillary artery, the superficial brachial artery (arteria brachialis superficialis), which is defined as the brachial artery that runs superficially to the median nerve. Totally, 130 cadaveric upper arms embalmed by classical formaldehyde technique from collections of the Department of Anatomy, Third Faculty of Medicine, Charles University in Prague, were macroscopically dissected with special focus on the branching arrangement of the axillary artery. The most distal part of the axillary artery (infrapectoral part) terminated in four cases as a bifurcation into two terminal branches: the superficial brachial artery and profunda brachii artery, denominated according to their relation to the median nerve. The profunda brachii artery primarily gave rise to the main branches of the infrapectoral part of the axillary artery. The superficial brachial artery descended to the cubital fossa where it assumed the usual course of the brachial artery in two cases and in the other two cases its branches (the radial and ulnar arteries) passed superficially to the flexors. The incidence of the superficial brachial artery in our study was 5% of cases. The reported incidence is a bit contradictory, from 0.12% to 25% of cases. The anatomical knowledge of the axillary region is of crucial importance for neurosurgeons and specialists using the radiodiagnostic techniques, particularly in cases involving traumatic injuries. The improved knowledge would allow more accurate diagnostic interpretations and surgical treatment.
Citations
Downloads
Additional Files
Published
How to Cite
Accepted 2017-11-01
Published 2011-02-20









