Impact of chemoradiotherapy on vaginal and sexual function of patients with FIGO IIb cervical cancer
DOI:
https://doi.org/10.17305/bjbms.2011.2628Keywords:
sexual function, vaginal function, chemoradiotherapy, cervical cancerAbstract
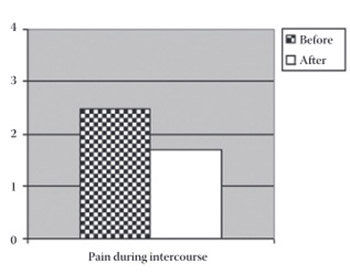
The opinion regarding sexual and vaginal function of patients with advanced cervical cancer treated primarily by chemoradiotherapy has still not been formed, mainly due to inappropriate methodology as the control group was comprised of healthy women. The aim of this study is to, by means of interview, evaluate vaginal and sexual function of patients with advanced cervical cancer before and after chemoradiotherapy and compare the results. A number of 35 patients were irradiated by teleradiotherapy dose of 45 Gy in 25 fractions over 5 weeks to the pelvis and additional 20-24 Gy in 4-6 fractions were given by intracavitary HDR brachytherapy. Patients received 40 mg/m2 of cisplatin once a week, which is a total of 4-6 cycles of cisplatin. Patients answered the questions in a form of a questionnaire specifically created for cervical cancer (EORTC-QLQ-Cx 24), for the period immediately before diagnosed cervical cancer (thus being a control group). They also answered the same questions for the period starting 12 months after the completion of concomitant chemoradiotherapy, and were an experimental group at the time. For the testing of statistical significance of differences among the examined groups parameter and non-parameter tests were used (the Wilcoxon signed ranks test and Student’s t-test). The difference p<0.05 was considered statistically significant. Vaginal problems of patients after chemoradiotherapy were statistically reduced (44 versus 0; p<0.0001). There is no statistical significance in the vaginal function among the analyzed groups but weaker pain during intercourse was registered after chemoradiotherapy (p=0.009). After chemoradiotherapy, patients’ vaginal function is extremely improved whereas there is no difference in the sexual function. Pain during intercourse is statistically reduced after chemoradiotherapy.
Citations
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2017-11-02
Published 2011-02-20









