Analysis of long non-coding RNA (lncRNA) expression in hepatitis B patients
DOI:
https://doi.org/10.17305/bjbms.2018.2800Keywords:
HBV, lncRNA, chronic hepatitis B, inactive HBsAg carrier, resolved hepatitis BAbstract
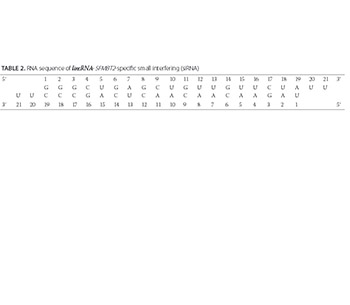
Long non-coding RNAs (lncRNAs) have been implicated in numerous biological processes, including epigenetic regulation, cell-cycle control, and transcriptional/translational regulation of gene expression. Differential expression of lncRNAs and disruption of the regulatory processes are recognized as critical steps in cancer development. The role of lncRNAs in hepatitis B virus (HBV) infection is not well understood. Here we analyzed the expression of 135 lncRNAs in plasma samples of 82 HBV patients (classified as chronic patients, inactive carriers, or resolved patients) at diagnosis and at 12 months of treatment in relation to control group (81 healthy volunteers). We also investigated the effect of small interfering RNA (siRNA)-mediated silencing of lincRNA-SFMBT2 on HBV-positive human liver cancer cell line. lncRNA expression was analyzed by quantitative reverse transcription-polymerase chain reaction (qRT-PCR). Chemically synthesized siRNAs were transfected into the cell lines using Lipofectamine 2000 Reagent (Thermo Fisher Scientific). HBV DNA and HBsAg and HBeAg were detected in transfected cultures by real-time PCR and ELISA, respectively, using commercial kits. We observed changes in lncRNA expression in all three HBV groups, compared to control group. Most notably, the expression of anti-NOS2A, lincRNA-SFMBT2, and Zfhx2as was significantly increased and expression of Y5 lncRNA was decreased in chronic HBV patients. A decreased Y5 expression and increased lincRNA-SFMBT2 expression were observed in inactive HBsAg carriers. The expression of HOTTIP, MEG9, and PCAT-32 was increased in resolved HBV patients, and no significant change in the expression of Y5 was observed, compared to control group. siRNA-mediated inhibition of lincRNA-SFMBT2 decreased the level of HBV DNA in human liver cancer cells. Further research is needed to confirm the prognostic as well as therapeutic role of these lncRNAs in HBV patients.
Citations
Downloads
References
Yuen MF, Hou JL, Chutaputti A, Asia Pacific Working Party on Prevention of Hepatocellular C. Hepatocellular carcinoma in the Asia pacific region. J Gastroenterol Hepatol 2009;24(3):346-53. https://doi.org/10.1111/j.1440-1746.2009.05784.x.
Kapranov P, Cheng J, Dike S, Nix DA, Duttagupta R, Willingham AT, et al. RNA maps reveal new RNA classes and a possible function for pervasive transcription. Science 2007;316(5830):1484-8. https://doi.org/10.1126/science.1138341.
Spizzo R, Almeida MI, Colombatti A, Calin GA. Long non-coding RNAs and cancer: A new frontier of translational research? Oncogene 2012;31(43):4577-87. https://doi.org/10.1038/onc.2011.621.
Ponting CP, Oliver PL, Reik W. Evolution and functions of long noncoding RNAs. Cell 2009;136(4):629-41. https://doi.org/10.1016/j.cell.2009.02.006.
Derrien T, Johnson R, Bussotti G, Tanzer A, Djebali S, Tilgner H, et al. The GENCODE v7 catalog of human long noncoding RNAs: Analysis of their gene structure, evolution, and expression. Genome Res 2012;22:1775-89. https://doi.org/10.1101/gr.132159.111.
Deng G, Sui G. Noncoding RNA in oncogenesis: A new era of identifying key players. Int J Mol Sci 2013;14(9):18319-49. https://doi.org/10.3390/ijms140918319.
Jeon Y, Sarma K, Lee JT. New and Xisting regulatory mechanisms of X chromosome inactivation. Curr Opin Genet Dev 2012;22(2):62-71. https://doi.org/10.1016/j.gde.2012.02.007.
Mattick JS, Amaral PP, Dinger ME, Mercer TR, Mehler MF. RNA regulation of epigenetic processes. Bioessays 2009;31(1):51-9. https://doi.org/10.1002/bies.080099.
Orom UA, Derrien T, Beringer M, Gumireddy K, Gardini A, Bussotti G, et al. Long noncoding RNAs with enhancer-like function in human cells. Cell 2010;143(1):46-58. https://doi.org/10.1016/j.cell.2010.09.001.
Rando TA, Chang HY. Aging, rejuvenation, and epigenetic reprogramming: Resetting the aging clock. Cell 2012;148(1-2):46-57. https://doi.org/10.1016/j.cell.2012.01.003.
Wapinski O, Chang HY. Long noncoding RNAs and human disease. Trends Cell Biol 2011;21(6):354-61. https://doi.org/10.1016/j.tcb.2011.04.001.
Gibb EA, Brown CJ, Lam WL. The functional role of long non-coding RNA in human carcinomas. Mol Cancer 2011;10:38. https://doi.org/10.1186/1476-4598-10-38.
Perz JF, Armstrong GL, Farrington LA, Hutin YJ, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol 2006;45(4):529-38. https://doi.org/10.1016/j.jhep.2006.05.013.
El-Serag HB. Hepatocellular carcinoma. N Engl J Med 2011;365(12):1118-27. https://doi.org/10.1056/NEJMra1001683.
Venook AP, Papandreou C, Furuse J, de Guevara LL. The incidence and epidemiology of hepatocellular carcinoma: A global and regional perspective. Oncologist 2010;15(Suppl 4):5-13. https://doi.org/10.1634/theoncologist.2010-S4-05.
Tsai WL, Chung RT. Viral hepatocarcinogenesis. Oncogene 2010;29(16):2309-24. https://doi.org/10.1038/onc.2010.36.
Feitelson MA, Reis HM, Tufan NL, Sun B, Pan J, Lian Z. Putative roles of hepatitis B x antigen in the pathogenesis of chronic liver disease. Cancer Lett 2009;286(1):69-79. https://doi.org/10.1016/j.canlet.2008.12.010.
Ringelhan M, Protzer U. Oncogenic potential of hepatitis B virus encoded proteins. Curr Opin Virol 2015;14:109-15. https://doi.org/10.1016/j.coviro.2015.08.015.
Tang H, Oishi N, Kaneko S, Murakami S. Molecular functions and biological roles of hepatitis B virus x protein. Cancer Sci 2006;97(10):977-83.
https://doi.org/10.1111/j.1349-7006.2006.00299.x.
Fu S, Li N, Zhou PC, Huang Y, Zhou RR, Fan XG. Detection of HBV DNA and antigens in HBsAg-positive patients with primary hepatocellular carcinoma. Clin Res Hepatol Gastroenterol 2017;41(4):415-23. https://doi.org/10.1016/j.clinre.2017.01.009.
Amaral PP, Clark MB, Gascoigne DK, Dinger ME, Mattick JS. lncRNAdb: A reference database for long noncoding RNAs. Nucleic Acids Res 2011;39(Database issue):D146-51. https://doi.org/10.1093/nar/gkq1138.
He H, Nagy R, Liyanarachchi S, Jiao H, Li W, Suster S, et al. A susceptibility locus for papillary thyroid carcinoma on chromosome 8q24. Cancer Res 2009;69(2):625-31. https://doi.org/10.1158/0008-5472.CAN-08-1071.
Korneev SA, Korneeva EI, Lagarkova MA, Kiselev SL, Critchley G, O'Shea M. Novel noncoding antisense RNA transcribed from human anti-NOS2A locus is differentially regulated during neuronal differentiation of embryonic stem cells. RNA 2008;14(10):2030-7. https://doi.org/10.1261/rna.1084308.
Guidotti LG, McClary H, Loudis JM, Chisari FV. Nitric oxide inhibits hepatitis B virus replication in the livers of transgenic mice. J Exp Med 2000;191(7):1247-52. https://doi.org/10.1084/jem.191.7.1247.
Mourtada-Maarabouni M, Pickard MR, Hedge VL, Farzaneh F, Williams GT. GAS5, a non-protein-coding RNA, controls apoptosis and is downregulated in breast cancer. Oncogene 2009;28(2):195-208. https://doi.org/10.1038/onc.2008.373.
Chang L, Li C, Lan T, Wu L, Yuan Y, Liu Q, et al. Decreased expression of long non-coding RNA GAS5 indicates a poor prognosis and promotes cell proliferation and invasion in hepatocellular carcinoma by regulating vimentin. Mol Med Rep 2016;13(2):1541-50. https://doi.org/10.3892/mmr.2015.4716.
Ariel I, Miao HQ, Ji XR, Schneider T, Roll D, de Groot N, et al. Imprinted H19 oncofetal RNA is a candidate tumour marker for hepatocellular carcinoma. Mol Pathol 1998;51(1):21-5. https://doi.org/10.1136/mp.51.1.21.
Kim KS, Lee YI. Biallelic expression of the H19 and IGF2 genes in hepatocellular carcinoma. Cancer Lett 1997;119(2):143-8. https://doi.org/10.1016/S0304-3835(97)00264-4.
Matouk IJ, DeGroot N, Mezan S, Ayesh S, Abu-lail R, Hochberg A, et al. The H19 non-coding RNA is essential for human tumor growth. PLoS One 2007;2(9):e845. https://doi.org/10.1371/journal.pone.0000845.
Iizuka N, Oka M, Yamada-Okabe H, Mori N, Tamesa T, Okada T, et al. Comparison of gene expression profiles between hepatitis B virus- and hepatitis C virus-infected hepatocellular carcinoma by oligonucleotide microarray data on the basis of a supervised learning method. Cancer Res 2002;62(14):3939-44.
Berteaux N, Aptel N, Cathala G, Genton C, Coll J, Daccache A, et al. A novel H19 antisense RNA overexpressed in breast cancer contributes to paternal IGF2 expression. Mol Cell Biol 2008;28(22):6731-45. https://doi.org/10.1128/MCB.02103-07.
Jiang YJ, Bikle DD. LncRNA profiling reveals new mechanism for VDR protection against skin cancer formation. J Steroid Biochem Mol Biol 2014;144(Pt A):87-90. https://doi.org/10.1016/j.jsbmb.2013.11.018.
Hao Y, Crenshaw T, Moulton T, Newcomb E, Tycko B. Tumour-suppressor activity of H19 RNA. Nature 1993;365:764-7. https://doi.org/10.1038/365764a0.
Pollard KS, Salama SR, Lambert N, Lambot MA, Coppens S, Pedersen JS, et al. An RNA gene expressed during cortical development evolved rapidly in humans. Nature 2006;443(7108):167-72. https://doi.org/10.1038/nature05113.
Liu H, Li J, Koirala P, Ding X, Chen B, Wang Y, et al. Long non-coding RNAs as prognostic markers in human breast cancer. Oncotarget 2016;7(15):20584-96. https://doi.org/10.18632/oncotarget.7828.
Chen X, Yan CC, Zhang X, You ZH. Long non-coding RNAs and complex diseases: From experimental results to computational models. Brief Bioinform 2017;18(4):558-76. https://doi.org/10.1093/bib/bbw060.
Johnson R, Richter N, Jauch R, Gaughwin PM, Zuccato C, Cattaneo E, et al. Human accelerated region 1 noncoding RNA is repressed by REST in Huntington's disease. Physiol Genomics 2010;41(3):269-74. https://doi.org/10.1152/physiolgenomics.00019.2010.
Zhou G, Du T, Roizman B. The role of the CoREST/REST repressor complex in herpes simplex virus 1 productive infection and in latency. Viruses 2013;5(5):1208-18. https://doi.org/10.3390/v5051208.
Wu L, Zhang L, Zheng S. Role of the long non-coding RNA HOTAIR in hepatocellular carcinoma. Oncol Lett 2017;14(2):1233-9. https://doi.org/10.3892/ol.2017.6312.
Zhang X, Lian Z, Padden C, Gerstein MB, Rozowsky J, Snyder M, et al. A myelopoiesis-associated regulatory intergenic noncoding RNA transcript within the human HOXA cluster. Blood 2009;113(11):2526-34. https://doi.org/10.1182/blood-2008-06-162164.
Wan L, Kong J, Tang J, Wu Y, Xu E, Lai M, et al. HOTAIRM1 as a potential biomarker for diagnosis of colorectal cancer functions the role in the tumour suppressor. J Cell Mol Med 2016;20(11):2036-44. https://doi.org/10.1111/jcmm.12892.
Wang KC, Yang YW, Liu B, Sanyal A, Corces-Zimmerman R, Chen Y, et al. A long noncoding RNA maintains active chromatin to coordinate homeotic gene expression. Nature 2011;472(7341):120-4. https://doi.org/10.1038/nature09819.
Quagliata L, Matter MS, Piscuoglio S, Arabi L, Ruiz C, Procino A, et al. Long noncoding RNA HOTTIP/HOXA13 expression is associated with disease progression and predicts outcome in hepatocellular carcinoma patients. Hepatology 2014;59(3):911-23. https://doi.org/10.1002/hep.26740.
Sonkoly E, Bata-Csorgo Z, Pivarcsi A, Polyanka H, Kenderessy-Szabo A, Molnar G, et al. Identification and characterization of a novel, psoriasis susceptibility-related noncoding RNA gene, PRINS. J Biol Chem 2005;280(25):24159-67. https://doi.org/10.1074/jbc.M501704200.
Vincent JB, Petek E, Thevarkunnel S, Kolozsvari D, Cheung J, Patel M, et al. The RAY1/ST7 tumor-suppressor locus on chromosome 7q31 represents a complex multi-transcript system. Genomics. 2002;80(3):283-94. https://doi.org/10.1006/geno.2002.6835.
Malik KT, Wallace JI, Ivins SM, Brown KW. Identification of an antisense WT1 promoter in intron 1: Implications for WT1 gene regulation. Oncogene 1995;11(8):1589-95.
Dallosso AR, Hancock AL, Malik S, Salpekar A, King-Underwood L, Pritchard-Jones K, et al. Alternately spliced WT1 antisense transcripts interact with WT1 sense RNA and show epigenetic and splicing defects in cancer. RNA 2007;13(12):2287-99. https://doi.org/10.1261/rna.562907.
Du T, Zhang B, Zhang S, Jiang X, Zheng P, Li J, et al. Decreased expression of long non-coding RNA WT1-AS promotes cell proliferation and invasion in gastric cancer. Biochim Biophys Acta 2016;1862(1):12-9. https://doi.org/10.1016/j.bbadis.2015.10.001.
Lerner MR, Boyle JA, Hardin JA, Steitz JA. Two novel classes of small ribonucleoproteins detected by antibodies associated with lupus erythematosus. Science 1981;211(4480):400-2. https://doi.org/10.1126/science.6164096.
Zhang AT, Langley AR, Christov CP, Kheir E, Shafee T, Gardiner TJ, et al. Dynamic interaction of Y RNAs with chromatin and initiation proteins during human DNA replication. J Cell Sci 2011;124(Pt 12):2058-69. https://doi.org/10.1242/jcs.086561.
Christov CP, Trivier E, Krude T. Noncoding human Y RNAs are overexpressed in tumours and required for cell proliferation. Br J Cancer 2008;98(5):981-8. https://doi.org/10.1038/sj.bjc.6604254.
Dhahbi JM, Spindler SR, Atamna H, Boffelli D, Mote P, Martin DI. 5'-YRNA fragments derived by processing of transcripts from specific YRNA genes and pseudogenes are abundant in human serum and plasma. Physiol Genomics 2013;45(21):990-8. https://doi.org/10.1152/physiolgenomics.00129.2013.
Dhahbi JM, Spindler SR, Atamna H, Boffelli D, Martin DI. Deep sequencing of serum small RNAs identifies patterns of 5' tRNA half and YRNA fragment expression associated with breast cancer. Biomark Cancer 2014;6:37-47. https://doi.org/10.4137/BIC.S20764.
Victoria Martinez B, Dhahbi JM, Nunez Lopez YO, Lamperska K, Golusinski P, Luczewski L, et al. Circulating small non-coding RNA signature in head and neck squamous cell carcinoma. Oncotarget 2015;6(22):19246-63. https://doi.org/10.18632/oncotarget.4266.
Subramanian M, Jones MF, Lal A. Long non-coding RNAs embedded in the Rb and p53 pathways. Cancers (Basel) 2013;5(4):1655-75. https://doi.org/10.3390/cancers5041655.
Loewer S, Cabili MN, Guttman M, Loh YH, Thomas K, Park IH, et al. Large intergenic non-coding RNA-RoR modulates reprogramming of human induced pluripotent stem cells. Nat Genet 2010;42(12):1113-7. https://doi.org/10.1038/ng.710.
Takahashi K, Yan IK, Kogure T, Haga H, Patel T. Extracellular vesicle-mediated transfer of long non-coding RNA ROR modulates chemosensitivity in human hepatocellular cancer. FEBS Open Bio 2014;4:458-67. https://doi.org/10.1016/j.fob.2014.04.007.
Downloads
Additional Files
Published
How to Cite
Accepted 2018-02-17
Published 2018-05-20









