p16/Ki-67 dual staining has a better accuracy than human papillomavirus (HPV) testing in women with abnormal cytology under 30 years old
DOI:
https://doi.org/10.17305/bjbms.2018.3560Keywords:
Human papillomavirus, immunocytochemistry, p16/Ki-67 dual staining, HPV genotypingAbstract
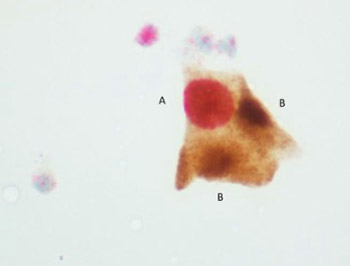
Due to a high rate of transient human papillomavirus (HPV) infection, HPV genotyping has a low specificity for high-grade cervical lesions, especially in young women. p16/Ki-67 dual immunocytochemical staining can also be used for the detection of oncogenic changes in cervical cells. Our aim was to compare the performance of p16/Ki-67 dual staining and HPV genotyping in the detection of high-grade cervical lesions in patients with atypical squamous cells of undetermined significance (ASCUS)/low-grade squamous intraepithelial lesion (LSIL) on Pap smear. We retrospectively analyzed 310 patients with ASCUS/LSIL on Pap smear, who underwent colposcopy. Among these, 161 patients with suspected lesions detected by colposcopy were referred for biopsy. HPV genotyping by LINEAR ARRAY HPV Genotyping Test (CE-IVD) and p16/Ki-67 dual staining by CINtec PLUS Cytology kit was performed prior to cervical biopsy. The overall sensitivity and specificity of HPV genotyping for the detection of cervical intraepithelial neoplasia (CIN) 2-3 was 79% and 72%, respectively in patients with ASCUS, and 85% and 64%, respectively in patients with LSIL. For p16/Ki-67 test, sensitivity and specificity rate was 66% and 93%, respectively in ASCUS and 59% and 79%, respectively in LSIL group. The specificity of p16/Ki-67 staining was significantly higher in both groups in patients aged <30 years compared to patients >30 years old (p < 0.001). Our results showed that p16/Ki-67 dual staining has a higher specificity compared to HPV genotyping, especially in patients under 30 years old. This indicates the usefulness of p16/Ki-67 testing in the triage of patients with ASCUS/LSIL and <30 years old, prior to referral for colposcopy and biopsy.
Citations
Downloads
Downloads
Additional Files
Published
How to Cite
Accepted 2018-05-22
Published 2019-11-08









