Frequency of the antipsychotic therapy acute side effects in the treatment of acute psychosis
DOI:
https://doi.org/10.17305/bjbms.2002.3577Keywords:
schizophrenia, antipsychotic agents, acute side effects, incidence, prevalence, intensity of side effectsAbstract
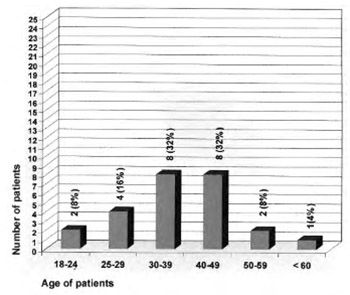
Antipsychotic drugs produce a wide spectrum of physiological actions. Some of these effects differ among the various classes of antipsychotics. This medications have indications in the treatment of acute psychotic disorders. The main goal of this investigation was to determine the incidence and prevalence of the neuroleptic therapy acute side effects. The reason for this epidemiological investigation performing was the lack of knowledge of the exact neuroleptic therapy side effects incidence. Qualitative study on this problem has not been performed yet. Antipsychotic therapy side effects prevalence rate according to the literature data is ranging from 24% to 74%. Different prevalence rate is a consequence of different antipsychotic drug usage, different drug administration method and different side effects identification. On account of all these facts, we put the hypothesis on the correlation between the antipsychotic therapy and occurred side effects. Our experiment included all patients hospitalised from December 31st 1999 to January 31st 2000 in Intensive Care Unit of Biological Psychiatry Department of Psychiatric Clinic in Sarajevo. All patients were divided in three groups according to the applied therapy. All of them met ICD-10 criteria for schizophrenia (F20-29). During our study the following examinations were performed: psychiatric interview, BRPS, scale of side effects, psychophysiological tests, general clinical impression, scale of appetite, carbon hydrate needs scale. Psychiatric and statistical evaluations were done as well. The evaluation of our examination is showing successful results in all groups of patients. The improvement of psychopathological symptoms was insignificant. Reported side effects were minimal with low incidence rate and relatively high prevalence rate. Statistical tests were calculated from the obtained data after what the null hypothesis was rejected. Consequently, an alternative hypothesis was confirmed and it indicated that the acute side effectsincidence and prevalence were within the range of expectation. Intensity of the recorded side effects was moderate to mild. On the basis of the obtained data, it has been concluded that applied antipsychotic agents did not induce more psychophysiological function impairments in the treated patients. Psychophysiological functions remained in physiological range limits and their changes were not significant. Neuroleptic therapy side effects were minimal, meaning no toxic signs or therapy discontinuations were recorded.
Citations
Downloads
Published
How to Cite
Accepted 2018-05-06
Published 2002-02-20









