Delirium following total joint replacement surgery
DOI:
https://doi.org/10.17305/bjbms.2018.3653Keywords:
Delirium, surgery, outcomes, total joint arthroplastyAbstract
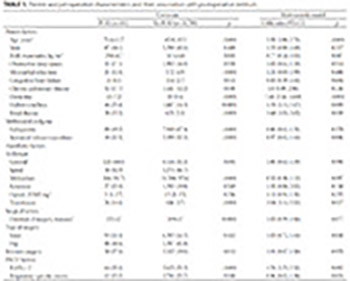
Postoperative delirium (POD) is a common complication associated with increased resource utilization, morbidity and mortality. Our institution screens all postsurgical patients for postoperative delirium. The study aim was to perform an automated interrogation of the electronic health records to estimate the incidence of and identify associated risk factors for POD following total joint arthroplasty (TJA). Adult patients who underwent TJA with a multimodal analgesia protocol, including peripheral nerve blockade, from 2008 through 2012, underwent automated chart review. POD was identified by routine nursing assessment and administrative billing codes. Of 11,970 patients, 181 (1.5%) were identified to have POD. Older age (odds ratio, 95% CI 2.20, 1.80–2.71 per decade, p < 0.001), dementia (7.44, 3.54–14.60, p < 0.001), diabetes mellitus (1.70, 1.1.5–2.47, p = 0.009), renal disease (1.68, 1.03–2.65, p = 0.039), blood transfusions (2.04, 1.14–3.52, p = 0.017), and sedation during anesthesia recovery (1.76, 1.23–2.51, p = 0.002) were associated with POD. Anesthetic management was not associated with POD risk. Patients who developed POD required greater healthcare resources. Dementia is strongly associated with POD. The association between POD and transfusions may reflect higher acuity patients or detrimental effect of blood. Postoperative sedation should be recognized as a warning sign of increased risk.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2018-06-27
Published 2019-02-12









