The effects of exercise on vascular markers and C-reactive protein among obese children and adolescents: An evidence-based review
DOI:
https://doi.org/10.17305/bjbms.2019.4345Keywords:
Exercise, vascular marker, inflammation, C-reactive protein, obese children and adolescentsAbstract
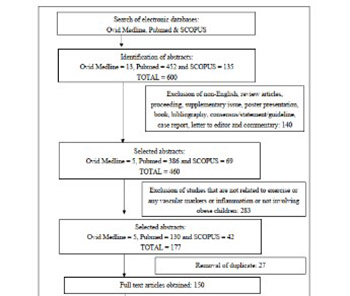
Numerous studies have evaluated the effects of exercise training on obese children and adolescents. However, the impact of aerobic and/or resistance exercise alone, without any other interventions, on vascular markers and C-reactive protein (CRP) in obese children and adolescents is still not clear. We performed a literature search in Ovid Medline, PubMed, and SCOPUS databases to identify articles on the effects of exercise on vascular markers and CRP among obese children and adolescents, published between January 2009 and May 2019. Only full-text articles in English that reported on the effect of aerobic and/or resistance exercise on the vascular markers pulse wave velocity (PWV), carotid intima-media thickness (CIMT), flow-mediated dilatation (FMD), augmentation index (AIx), or CRP in obese children and adolescents (5–19 years old) were included. The literature search identified 36 relevant articles; 9 articles that fulfilled all the inclusion criteria were selected by two independent reviewers. Aerobic exercise or a combination of aerobic and resistance exercise training significantly improved CIMT and PWV in obese children and adolescents in all studies in which they were measured (2 studies for PWV and 4 studies for CIMT). However, the effects of exercise on FMD and CRP levels were inconclusive, as only half of the studies demonstrated significant improvements (1/2 studies for FMD and 4/8 studies for CRP). The results of our review support the ability of exercise to improve vascular markers such as PWV and CIMT in obese children and adolescents. This finding is important as obesity is a modifiable risk factor of cardiovascular disease (CVD), and exercise may help in reducing the future occurrence of CVD in this population.
Citations
Downloads
Downloads
Additional Files
Published
How to Cite
Accepted 2019-08-06
Published 2020-05-01









