The effects of mutational profiles on phenotypic presentation of myeloproliferative neoplasm subtypes in Bosnia: 18 year follow-up
DOI:
https://doi.org/10.17305/bjbms.2019.4391Keywords:
MPN, myeloproliferative neoplasm, JAK2, janus kinase 2, CALR, calreticulin, MPL, myeloproliferative leukemia virus, mutant allele burdenAbstract
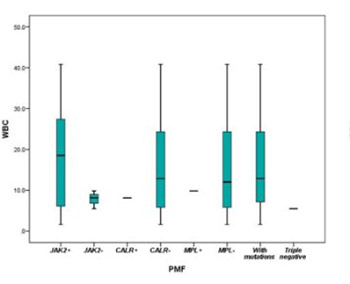
The identification of mutually exclusive somatic mutations shared among myeloproliferative neoplasm (MPN) subtypes has provided a powerful tool for studying disease evolution. Clinical features, gene mutations, and survival over 18 years were analyzed in MPN patients. One hundred thirty-eight MPN patients were subcategorized according to MPN subtypes: essential thrombocythemia (ET, n = 41), polycythemia vera (PV, n = 56), primary myelofibrosis (PMF, n = 10), and MPN unclassified (MPN-U, n = 31). Patient characteristics included clinical parameters, overall survival (OS), and mutational status of the Janus kinase 2 (JAK2), calreticulin (CALR), and myeloproliferative leukemia virus oncogene (MPL) genes. We compared hematologic and clinical features of JAK2V617F-ET vs. CALR-mutated ET vs. JAK2V617F-PV patients. JAK2V617F-patients had higher values of erythrocytes, hemoglobin, and hematocrit compared to CALR-mutated patients (p < 0.05). The mutant allele burden in JAK2V617F-PV and JAK2V617F-ET patients directly correlated with erythrocyte, hemoglobin, and hematocrit values, but it inversely correlated with platelet count. Thus, mutant allele burden was an indicator of the clinical phenotype in JAK2V617F-MPN patients. OS was not affected by the mutational status. In general, mutated JAK2, CALR, and MPL genes left specific hematological signatures.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2019-10-25
Published 2020-05-01









