Laryngeal tuberculosis in renal transplant recipients: A case report and review of the literature
DOI:
https://doi.org/10.17305/bjbms.2020.4448Keywords:
Laryngeal tuberculosis, kidney transplant, laryngeal leukoplakiaAbstract
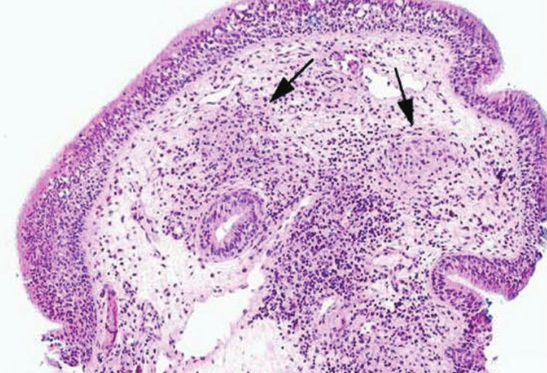
Renal allograft recipients are at greater risk of developing tuberculosis than the general population. A woman with a kidney transplant was admitted to our emergency department with high temperature, dysphonia, odynophagia, and asthenia. The final diagnosis was laryngeal tuberculosis. Multidisciplinary collaboration enabled accurate diagnosis and successful treatment. Laryngeal tuberculosis should be considered in renal allograft recipients with hoarseness. A more rapid diagnosis of tuberculosis in renal transplant recipients is desirable when the site involved, such as the larynx, exhibits specific manifestations and the patient exhibits specific symptoms. In these cases, prognosis is excellent, and with adequate treatment a complete recovery is often achieved.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2020 Fabrizio Cialente, Michele Grasso, Massimo Ralli, Marco de Vincentiis, Antonio Minni, Griselda Agolli, Michele Dello Spedale Venti, Mara Riminucci, Alessandro Corsi, Antonio Greco

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2020-02-20
Published 2020-08-03









