A three-dimensional computed tomography study to determine the ideal method for fluoroscopically-guided bone marrow aspiration from the iliac crest
DOI:
https://doi.org/10.17305/bjbms.2020.4744Keywords:
Mesenchymal stem cells, bone marrow aspirate, regenerative medicineAbstract
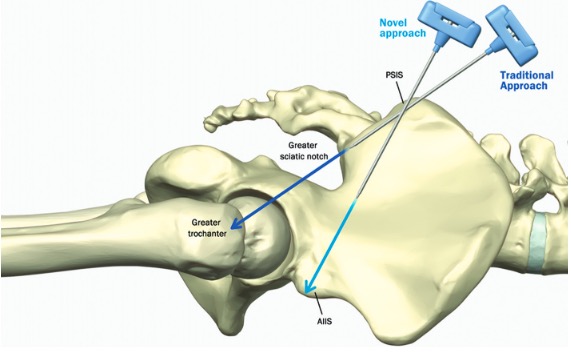
Bone marrow aspiration (BMA) through the iliac crest is potentially unsafe due to the vicinity of neurovascular structures in the greater sciatic notch. Our objective was to investigate the safety of a recently described BMA technique, specifically a trajectory from the posterior superior iliac spine (PSIS) to the anterior inferior iliac spine (AIIS). We conducted a chart review of 260 patients, analyzing three-dimensional reconstructed computed tomography images of the pelvis and sacrum to validate that this new approach offers a wide safety margin from the greater sciatic notch. Analysis of three-dimensional computed tomography scans demonstrated that the PSIS to AIIS trajectory never crossed the greater sciatic notch. The trajectory was noted to be at least one cm away from the greater sciatic notch in all measurements. The new trajectory entered the PSIS at 25.29 ± 4.34° (left side) and 24.93 ± 4.15° (right side) cephalad from the transverse plane, and 24.58 ± 4.99° (left side) and 24.56 ± 4.67° (right side) lateral from the mid-sagittal plane. The area of bone marrow encountered with the new approach was approximately 22.5 cm2. Utilizing the same CT scans, the trajectory from the traditional approach crossed the greater sciatic notch in all scans, highlighting the potential for violating the greater sciatic notch boundary and damaging important neurovascular structures. Statistically significant sex-related differences were identified in needle trajectory angles for both approaches. We conclude that based on this three-dimensional computed tomography study, a trajectory from the PSIS to the AIIS for BMA may offer a wide safety margin from the greater sciatic notch.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2020-05-10
Published 2021-06-01









