Respiratory depression in the post-anesthesia care unit: Mayo Clinic experience
DOI:
https://doi.org/10.17305/bjbms.2020.4816Keywords:
Respiratory depression, post-anesthesia care unit, ERASAbstract
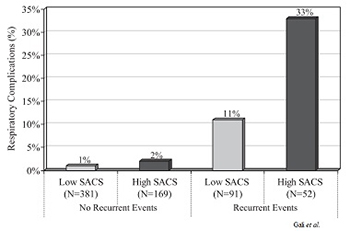
The anesthesia recovery is a complex physiologic process as systems recover from the effects of surgery and anesthesia. Inadequate recovery of respiratory physiology can lead to severe hypoxemia-induced end-organ damage and even death. Emerging evidence suggests that signs of respiratory depression during early anesthesia recovery may portend increased risk for future severe adverse events. This article briefly reviews the Mayo Clinic research experience and advances in clinical practice. From the implementation of a step-down model of discharge criteria in the post-anesthesia care unit (PACU), consisting of PACU nurses monitoring patients in predetermined periods for signs of respiratory depression, and delaying PACU discharge for patients who exhibit signs of respiratory depression, and early intervention in high-risk patients. Subsequent studies found that even a single episode of respiratory depression in the PACU was strongly associated with subsequent respiratory complications. Further, patient baseline characteristics found to be associated with respiratory depression included obstructive sleep apnea and low body weight, and surgical factors associated with increased risk included the use of preoperative sustained-release opioids, perioperative gabapentinoid use, higher intraoperative opioids, isoflurane as the volatile anesthetic, and longer surgical duration. Based in part of Mayo Clinic research, the FDA issued a warning in 2019 on gabapentinoids use and respiratory complications, increasing the recommended level of respiratory vigilance in patients using this medication. Understanding the complex nature of postoperative respiratory events requires a range of translational and clinical research and constant update of practice.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2020-05-12
Published 2021-04-01









