Prevalence, clinical features and prognosis of malignant solid tumors in infants: a 14-year study
DOI:
https://doi.org/10.17305/bjbms.2020.5121Keywords:
Infants, malignant solid tumors, clinical features, prognosisAbstract
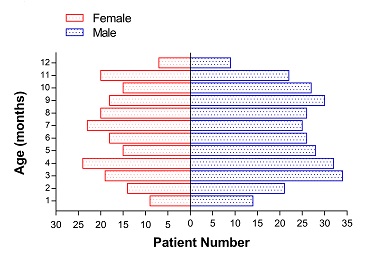
The onset of malignant solid tumors in infants is insidious and difficult to diagnose on time. The purpose of our study is to provide a theoretical basis for clinical diagnosis by retrospective analysis of the data in the past 14 years. Here, we retrospectively collected the clinical data of infants aged 0-12 months with malignant solid tumors in Beijing Tongren Hospital Affiliated to Capital Medical University from May 2005 to May 2019. The epidemiology, clinical characteristics, treatments and prognosis were statistically analyzed. A total of 496 infants (294 males and 202 females) with malignant solid tumors were analyzed. The main period of onset was 1-11 months. The most common tumor was retinoblastoma (RB, 51.8%), followed by hepatoblastoma (HB, 26.6%), neuroblastoma (NB, 10.5%), rhabdomyosarcoma (RMS, 3.4%), malignant renal tumors (3.2%), infantile fibrosarcoma (IFS, 1.6%), malignant teratoma (1.2%), Ewing’s sarcoma (ES, 0.8%), medulloblastoma (MB, 0.4%) and inflammatory myofibroblastic tumor (IMT, 0.4%). The median follow-up time was 32 months (range 2-162 months). The 1-year, 3-year, and 5-year overall survival of all patients were 97.3%, 89.2%, and 81.1%, respectively, and event-free survival was 94.7%, 84.8%, and 75.8%, respectively. In conclusion, as a special group, malignant solid tumors in infants are complex, heterogeneous, and relatively rare. The prognosis of RB, HB, NB, RMS, malignant renal tumors, IFS, malignant teratoma, ES, MB, and IMT, were excellent duo to timely diagnosis and rational treatment.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2020-11-30
Published 2021-10-01









