Sirtuin 1 rs7069102 polymorphism is associated with diabetic nephropathy in patients with type 2 diabetes mellitus
DOI:
https://doi.org/10.17305/bjbms.2020.5368Keywords:
SIRT1, rs7069102, diabetic nephropathy, type 2 diabetes mellitus, association studyAbstract
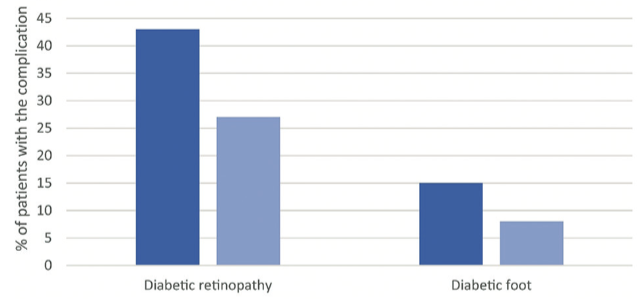
The global prevalence for diabetes mellitus nearly doubled from 4.7% in 1980 to 8.5% in 2014. Sirtuin 1 (SIRT1) is an NAD+-dependent deacetylase that is expressed in a variety of tissues. It modifies proteins that participate in DNA repair, stress, and inflammatory response. The aim of the study was to investigate the relationship between SIRT1 rs7069102 polymorphism and diabetic nephropathy (DN) in patients with type 2 diabetes mellitus (T2DM). In our retrospective association study, we included 724 Slovene (Caucasian) patients who have had T2DM for at least 10 years. We classified the participants into two groups, the first group was comprised of 301 patients with DN, and the second (control) group was comprised of 423 patients without DN. We analyzed the rs7069102 polymorphism using StepOne real-time polymerase chain reaction (PCR) System and TaqMan SNP Genotyping Assay. We found a statistically significant difference in the distribution of rs7069102 genotypes and alleles between the two groups. We used logistic regression analysis and adjusted for systolic pressure, arterial hypertension (AH), duration of AH, triglycerides, the value of HbA1c, carotid disease, diabetic foot, and diabetic retinopathy. Furthermore, we discovered that patients with the CC genotype are significantly more likely to develop DN according to both the codominant (odds ratio [OR] = 1.94; 95% confidence interval [CI] = 1.09-3.45; p = 0.02) and recessive (OR = 2.39; 95% CI = 1.12-5.08; p = 0.02) models of inheritance. We found a significant association between the SIRT1 rs7069102 polymorphism and DN in T2DM. We speculate that SIRT1 rs7069102 might be an interesting marker of DN.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2021 Jernej Letonja, Matej Završnik, Jana Makuc, Maja Šeruga, Ana Peterlin, Ines Cilenšek, Danijel Petrovič

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2021-01-27
Published 2021-10-01









