Predictive performance of CT for adverse outcomes among COVID-19 suspected patients: a two-center retrospective study
DOI:
https://doi.org/10.17305/bjbms.2020.5466Keywords:
COVID-19, pandemic, SARS virus, computed tomography, X-raysAbstract
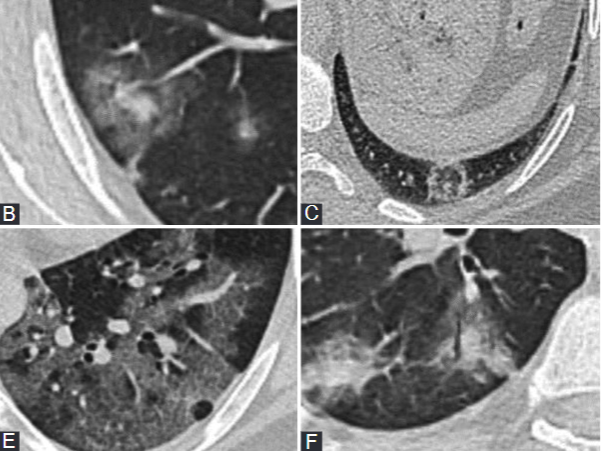
The aim of the study was to compare the performance of various computed tomography (CT) reporting tools, including zonal CT visual score (ZCVS), the number of involved lobes, and Radiological Society of North America (RSNA) categorization in predicting adverse outcomes among patients hospitalized due to the lower respiratory symptoms during the coronavirus disease 2019 (COVID-19) pandemic. A total of 405 patients admitted with severe respiratory symptoms who underwent a chest CT were enrolled. The primary adverse outcome was intensive care unit (ICU) admission of patients. Predictive performances of reporting tools were compared using the area under the receiver operating characteristic curves (AUC ROC). Among the 405 patients, 39 (9.63%) required ICU support during their hospital stay. At least two or more observers reported a typical and indeterminate COVID-19 pneumonia CT pattern according to RSNA categorization in 70% (285/405) of patients. Among these, 63% (179/285) had a positive polymerase chain reaction (PCR test for the SARS-CoV-2 virus. The median number of lobes involved according to CT was higher in patients who required ICU support (median interquartile range [IQR], 5[3; 5] vs. 3[0; 5]). The median ZCVS score was higher among the patients that subsequently required ICU support (median [IQR], 4[0; 12] vs. 13[5.75; 24]). The bootstrap comparisons of AUC ROC showed significant differences between reporting tools, and the ZCVS was found to be superior (AUC ROC, 71-75%). The ZCVS score at the first admission showed a linear and significant association with adverse outcomes among patients with the lower respiratory tract symptoms during the COVID-19 pandemic.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2021 Begümhan Baysal, Mahmut Bilal Dogan, Mutlu Gulbay, Mine Sorkun, Murathan Koksal, Aliye Bastug, Sumeyye Kazancioglu, Bahadir Orkun Ozbay, Sacit Icten, Ferhat Arslan, Yasemin Cag, Hurrem Bodur, Haluk Vahaboglu

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2021-02-08
Published 2021-12-01









