The value of routine measurement of serum calcitonin on insufficient, indeterminate, and suspicious thyroid nodule cytology
DOI:
https://doi.org/10.17305/bjbms.2021.5756Keywords:
Nodular thyroid disease, calcitonin, medullary thyroid cancer, cytologyAbstract
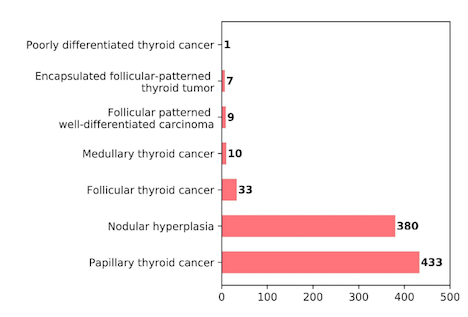
Routine calcitonin measurement in patients with nodular thyroid disease is rather controversial. The aim of this study was to evaluate the contribution of serum calcitonin measurement in the diagnostic evaluation of thyroid nodules with insufficient, indeterminate, or suspicious cytology. Out of 1668 patients who underwent thyroidectomy with the diagnosis of nodular thyroid disease and were screened, 873 patients with insufficient, indeterminate, or suspicious fine needle aspiration biopsy results were included in the study. From the total number of patients in this study, 10 (1.1%) were diagnosed as medullary thyroid cancer (MTC) using histopathology. The calcitonin level was detected to be above the assay-specific cut-off in 23 (2.6%) patients ranging between 6.5 - 4450 pg/mL. While hypercalcitoninemia was detected in all 10 MTC patients, a false positive elevation of serum calcitonin was detected in 13 patients (1.5%). Of the MTC group, 7 patients had cytology results that were suspicious for malignancy (Bethesda V), one patient’s cytology showed atypia of undetermined significance (Bethesda III) and two patient’s cytology results were suspicious for follicular neoplasm (Bethesda IV). Among the cases with non-diagnostic cytology (Bethesda I), none of the patients were diagnosed with MTC. In conclusion, routine serum calcitonin measurement can be performed in selected cases rather than in all nodular thyroid patients. While it is reasonable to perform routine calcitonin measurement in patients with Bethesda IV and Bethesda V, this measurement was not useful in Bethesda I patients. In Bethesda III patients, patient-based decisions can be made according to their calcitonin measurement.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2021-05-14
Published 2022-02-01









