Construction and validation of prognostic nomogram for metaplastic breast cancer
DOI:
https://doi.org/10.17305/bjbms.2021.5911Keywords:
Metaplastic breast cancer, nomogram, overall survival, cancer-specific survivalAbstract
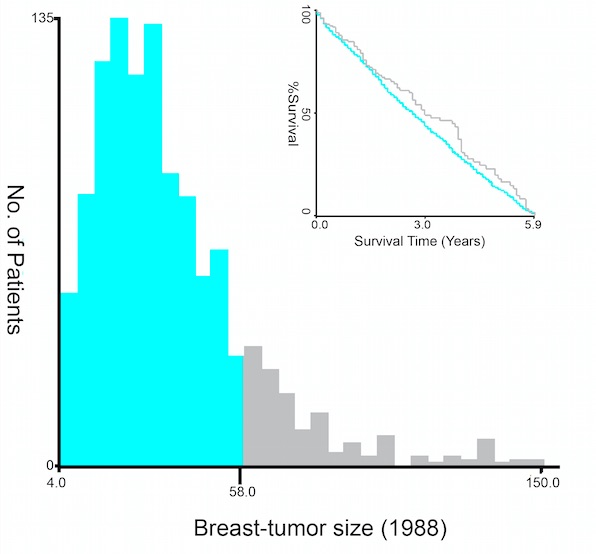
In this study we aimed to develop nomogram models for predicting the overall survival (OS) and cancer-specific survival (CSS) of patients with metaplastic breast cancer (MBC). Data of patients diagnosed with MBC from 1973 to 2015 were collected from the Surveillance, Epidemiology, and End Results (SEER) database. Univariate and multivariate Cox analyses were performed to identify independent prognostic factors for OS and CSS of MBC patients. The obtained prognostic variables were combined to construct nomogram models for predicting OS and CSS in patients with MBC. Model performance was evaluated using concordance index (C-index) and calibration plots. Data from 1125 patients were collected and divided into a training (750) and a validation (375) cohort. The multivariate Cox model identified age, TNM stage, tumor size, and radiotherapy as independent covariates associated with OS and CSS. The nomogram constructed based on these covariates demonstrated excellent accuracy in estimating 3-, and 5-year OS and CSS, with a C-index of 0.769 (95% CI, 0.731-0.808) for OS and 0.761 (95% CI, 0.713-0.809) for CSS in the training cohort. In the validation cohort, the nomogram-predicted C-index was 0.738 (95%CI, 0.676-0.800) for OS and 0.747 (95%CI, 0.667-0.827) for CSS. All calibration curves exhibited good consistency between predicted and actual survival. The nomogram models established in this study may enhance the accuracy of prognosis prediction and therefore may improve individualized assessment of survival risks and enable constructive therapeutic suggestions.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2021-05-31
Published 2022-02-01









