COVID-19 associated cranial nerve neuropathy: A systematic review
DOI:
https://doi.org/10.17305/bjbms.2021.6341Keywords:
Cranial nerves, nerve conduction, neuropathy, SARS-CoV-2, COVID-19, Guillain Barre syndromeAbstract
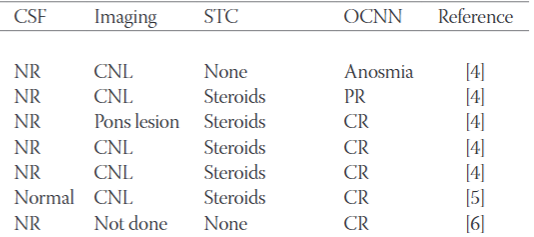
The involvement of cranial nerves is being increasingly recognised in COVID-19. This review aims to summarize and discuss the recent advances concerning the clinical presentation, pathophysiology, diagnosis, treatment, and outcomes of SARS-CoV-2 associated cranial nerve mononeuropathies or polyneuropathies. Therefore, a systematic review of articles from PubMed and Google Scholar was conducted. Altogether 36 articles regarding SARS-CoV-2 associated neuropathy of cranial nerves describing 56 patients were retrieved. Out of these 56 patients, cranial nerves were compromised without the involvement of peripheral nerves in 32 of the patients, while Guillain-Barre syndrome (GBS) with cranial nerve involvement was described in 24 patients. A single cranial nerve was involved either unilaterally or bilaterally in 36 patients, while in 19 patients multiple cranial nerves were involved. Bilateral involvement was more prevalent in the GBS group (n=11) as compared to the cohort with isolated cranial nerve involvement (n=5). Treatment of cranial nerve neuropathy included steroids (n=18), intravenous immunoglobulins (IVIG) (n=18), acyclovir/valacyclovir (n=3), and plasma exchange (n=1). The outcome was classified as “complete recovery” in 21 patients and as ”partial recovery” in 30 patients. One patient had a lethal outcome. In conclusion, any cranial nerve can be involved in COVID-19, but cranial nerves VII, VI, and III are the most frequently affected. The involvement of cranial nerves in COVID-19 may or may not be associated with GBS. In patients with cranial nerve involvement, COVID-19 infections are usually mild. Isolated cranial nerve palsy without GBS usually responds favorably to steroids. Cranial nerve involvement with GBS benefits from IVIG.
Citations
Downloads
Downloads
Additional Files
Published
Issue
Section
Categories
License
Copyright (c) 2021 Josef Finsterer

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Accepted 2021-08-05
Published 2022-02-01









