Dystrophin and the two related genetic diseases, Duchenne and Becker muscular dystrophies
DOI:
https://doi.org/10.17305/bjbms.2015.636Keywords:
Dystrophin, Becker muscular dystrophy, Duchenne muscular dystrophy, exon skipping, micro-dystrophinAbstract
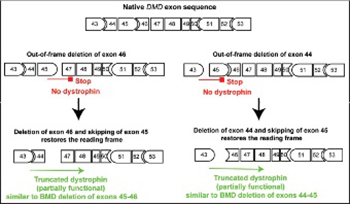
Mutations of the dystrophin DMD gene, essentially deletions of one or several exons, are the cause of two devastating and to date incurable diseases, Duchenne (DMD) and Becker (BMD) muscular dystrophies. Depending upon the preservation or not of the reading frame, dystrophin is completely absent in DMD, or present in either a mutated or a truncated form in BMD. DMD is a severe disease which leads to a premature death of the patients. Therapy approaches are evolving with the aim to transform the severe DMD in the BMD form of the disease by restoring the expression of a mutated or truncated dystrophin. These therapies are based on the assumption that BMD is a mild disease. However, this is not completely true as BMD patients are more or less severely affected and no molecular basis of this heterogeneity of the BMD form of the disease is yet understood. The aim of this review is to report for the correlation between dystrophin structures in BMD deletions in view of this heterogeneity and to emphasize that examining BMD patients in details is highly relevant to anticipate for DMD therapy effects.
Citations
Downloads
References
Koenig M, Beggs A, Moyer M, Scherpf S, Heindrich K, Bettecken T, et al. The molecular basis for Duchenne versus Becker muscular dystrophy: correlation of severity with type of deletion. Am J Hum Genet. 1989;45:498-506.
Koenig M, Hoffman EP, Bertelson CJ, Monaco AP, Feener C, Kunkel LM. Complete cloning of the Duchenne muscular dystrophy (DMD) cDNA and preliminary genomic organization of the DMD gene in normal and affected individuals. Cell. 1987 Jul 31;50:509-17.
Kenwrick S, Patterson M, Speer A, Fischbeck K, Davies K. Molecular analysis of the Duchenne muscular dystrophy region using pulsed field gel electrophoresis. Cell. 1987 Jan 30;48:351-7.
Flanigan KM, Dunn DM, von Niederhausern A, Soltanzadeh P, Gappmaier E, Howard MT, et al. Mutational spectrum of DMD mutations in dystrophinopathy patients: application of modern diagnostic techniques to a large cohort. Hum Mutat. 2009 Dec;30:1657-66.
Tuffery-Giraud S, Beroud C, Leturcq F, Yaou RB, Hamroun D, Michel-Calemard L, et al. Genotype-phenotype analysis in 2,405 patients with a dystrophinopathy using the UMD-DMD database: a model of nationwide knowledgebase. Hum Mutat. 2009 Jun;30:934-45.
Monaco A, Bertelson C, Liechti-Gallati S, Moser H, Kunkel L. An explanation for the phenotypic differences between patients bearing partial deletions of the DMD locus. Genomics. 1988;2:90-5.
Wein N, Alfano L, Flanigan KM. Genetics and Emerging Treatments for Duchenne and Becker Muscular Dystrophy. Pediatr Clin N Am. 2015;62(3):723-42.
Kohler M, Clarenbach CF, Boni L, Brack T, Russi EW, Bloch KE. Quality of life, physical disability, and respiratory impairment in Duchenne muscular dystrophy. Am J Respir Crit Care Med. 2005 Oct 15;172:1032-6.
Davies KE, Nowak KJ. Molecular mechanisms of muscular dystrophies: old and new players. Nat Rev Mol Cell Biol. 2006 Oct;7:762-73.
Rahimov F, Kunkel LM. The cell biology of disease: cellular and molecular mechanisms underlying muscular dystrophy. J Cell Biol. 2013 May 13;201:499-510.
Bushby KM, Gardner-Medwin D. The clinical, genetic and dystrophin characteristics of Becker muscular dystrophy. I. Natural history. J Neurol. 1993 Feb;240:98-104.
Bushby KM, Gardner-Medwin D, Nicholson LV, Johnson MA, Haggerty ID, Cleghorn NJ, et al. The clinical, genetic and dystrophin characteristics of Becker muscular dystrophy. II. Correlation of phenotype with genetic and protein abnormalities. J Neurol. 1993 Feb;240:105-12.
Petrof BJ, Shrager JB, Stedmann HH, Kelly AM, Sweeney HL. Dystrophin protects the sarcolemma from stresses developed during muscle contraction. Proceedings of the National Academy of Sciences, USA. 1993;90:3710-4.
Neri M, Torelli S, Brown S, Ugo I, Sabatelli P, Merlini L, et al. Dystrophin levels as low as 30% are sufficient to avoid muscular dystrophy in the human. Neuromuscul Disord. 2007 Dec;17:913-8.
Anthony K, Cirak S, Torelli S, Tasca G, Feng L, Arechavala-Gomeza V, et al. Dystrophin quantification and clinical correlations in Becker muscular dystrophy: implications for clinical trials. Brain. 2011 Dec;134:3544-56.
Aartsma-Rus A. Dystrophin analysis in clinical trials. Journal of Neuromuscular diseases. 2014;1:41-53.
Dubowitz V, Cohn RD. Dystrophin and Duchenne dystrophy. Neuromuscul Disord. 2015 May;25:361-2.
Ervasti J, Campbell K. Dystrophin and the membrane skeleton. Curr Op Cell Biol. 1993;5:82-7.
Le Rumeur E, Winder SJ, Hubert JF. Dystrophin: More than just the sum of its parts. Biochim Biophys Acta. 2010 Sep;1804:1713-22.
Levine BA, Moir AJG, Patchell VB, Perry SV. Binding sites involved in the interaction of actin with the N-terminal region of dystrophin. FEBS Letters. 1992;298:44-8.
Keep NH, Norwood FLM, Moores CA, Winder SJ, Kendrick-Jones J. The 2.0 A Structure of the Second Calponin Homology Domain from the Actin-binding Region of the Dystrophin Homologue Utrophin. J Mol Biol. 1999;285:1257-64.
Norwood F, Sutherland-Smith A, Keep N, Kendrick-Jones J. The structure of the N-terminal actin-binding domain of human dystrophin and how mutations in this domain may cause Duchenne or Becker muscular dystrophy. Structure. 2000;8:481-91.
Koenig M, Kunkel LM. Detailed analysis of the repeat domain of dystrophin reveals four potential hinge segments that may confer flexibility. J Biol Chem. 1990;265:4560-6.
Amann KJ, Renley BA, Ervasti JM. A Cluster of Basic Repeats in the Dystrophin Rod Domain Binds F-actin through an Electrostatic Interaction. J Biol Chem. 1998;273:28419-23.
Bhosle RC, Michele DE, Campbell KP, Li Z, Robson RM. Interactions of intermediate filament protein synemin with dystrophin and utrophin. Biochem Biophys Res Commun. 2006 Aug 4;346:768-77.
Stone MR, O'Neill A, Catino D, Bloch RJ. Specific interaction of the actin-binding domain of dystrophin with intermediate filaments containing keratin 19. Mol Biol Cell. 2005 Sep;16:4280-93.
Prins KW, Humston JL, Mehta A, Tate V, Ralston E, Ervasti JM. Dystrophin is a microtubule-associated protein. J Cell Biol. 2009 Aug 10;186:363-9.
Belanto JJ, Mader TL, Eckhoff MD, Strandjord DM, Banks GB, Gardner MK, et al. Microtubule binding distinguishes dystrophin from utrophin. Proc Natl Acad Sci U S A. 2014 Apr 15;111:5723-8.
Lai Y, Thomas GD, Yue Y, Yang HT, Li D, Long C, et al. Dystrophins carrying spectrin-like repeats 16 and 17 anchor nNOS to the sarcolemma and enhance exercise performance in a mouse model of muscular dystrophy. J Clin Invest. 2009 Mar;119:624-35.
Lai Y, Zhao J, Yue Y, Duan D. alpha2 and alpha3 helices of dystrophin R16 and R17 frame a microdomain in the alpha1 helix of dystrophin R17 for neuronal NOS binding. Proc Natl Acad Sci U S A. 2013 Nov 26;110:525-30.
Giudice E, Molza A-E, Laurin Y, Nicolas A, Le Rumeur E, Delalande O. Molecular clues to the dystrophin–nNOS interaction: a theoretical approach. Biochemistry. 2013;52:7777-84.
Yamashita K, Suzuki A, Satoh Y, Ide M, Amano Y, Masuda-Hirata M, et al. The 8th and 9th tandem spectrin-like repeats of utrophin cooperatively form a functional unit to interact with polarity-regulating kinase PAR-1b. Biochem Biophys Res Commun. 2010 Nov 26;391:812–7.
Le Rumeur E, Fichou Y, Pottier S, Gaboriau F, Rondeau-Mouro C, Vincent M, et al. Interaction of dystrophin rod domain with membrane phospholipids: evidence of a close proximity between tryptophan residues and lipids. J Biol Chem. 2003;278:5993-6001.
Legardinier S, Hubert J-F, Le Bihan O, Tascon C, Rocher C, Raguénès-Nicol C, et al. Sub-domains of the dystrophin rod domain display contrasting lipid-binding and stability properties. Biochim Biophys Acta. 2008;1784:672-82.
Legardinier S, Raguénès-Nicol C, Tascon C, Rocher C, Hardy S, Hubert JF, et al. Mapping of the lipid-binding and stability properties of the central rod domain of human dystrophin. J Mol Biol. 2009;389:546-58.
Campbell K, Kahl S. Association of dystrophin and an integral membrane glycoprotein. Nature. 1989;338:259-62.
Ervasti J, Campbell K. A Role for the Dystrophin-Glycoprotein Complex as aTransmembrane Linker between Laminin and Actin. J Cell Biol. 1993;122:809-23.
Huang X, Poy F, Zhang R, Joachimiak A, Sudol M, Eck MJ. Structure of a WW domain containing fragment of dystrophin in complex with beta-dystroglycan. Nat Struct Biol. 2000 Aug;7:634-8.
Hnia K, Zouiten D, Cantel S, Chazalette D, Hugon G, Fehrentz JA, et al. ZZ domain of dystrophin and utrophin: topology and mapping of a beta-dystroglycan interaction site. Biochem J. 2007 Feb 1;401:667-77.
Rezniczek GA, Konieczny P, Nikolic B, Reipert S, Schneller D, Abrahamsberg C, et al. Plectin 1f scaffolding at the sarcolemma of dystrophic (mdx) muscle fibers through multiple interactions with beta-dystroglycan. J Cell Biol. 2007 Mar 26;176:965-77.
Ayalon G, Davis JQ, Scotland PB, Bennett V. An ankyrin-based mechanism for functional organization of dystrophin and dystroglycan. Cell. 2008 Dec 26;135:1189-200.
Sadoulet-Puccio H, Rajala M, Kunkel L. Dystrobrevin and dystrophin: An interaction through coiled-coil motifs. Proc Natl Acad Sci USA. 1997;94:12413-8.
Newey SE, Benson MA, Ponting CP, Davies KE, Blake DJ. Alternative splicing of dystrobrevin regulates the stoichiometry of syntrophin binding to the dystrophin protein complex. Curr Biol. 2000 Oct 19;10:1295-8.
Zubrzycka-Gaarn EE, Bulman DE, Karpati G, Burghes AH, Belfall B, Klamut HJ, et al. The Duchenne muscular dystrophy gene product is localized in sarcolemma of human skeletal muscle. Nature. 1988 Jun 2;333:466-9.
Jaka O, Casas-Fraile L, Lopez de Munain A, Saenz A. Costamere proteins and their involvement in myopathic processes. Expert Rev Mol Med. 2015;17:e12.
Ervasti JM. Costameres: the Achilles' heel of Herculean muscle. J Biol Chem. 2003 Apr 18;278:13591-4.
Bloch RJ, Capetanaki Y, O'Neill A, Reed P, Williams MW, Resneck WG, et al. Costameres: repeating structures at the sarcolemma of skeletal muscle. Clin Orthop Relat Res. 2002 Oct:S203-10.
Bloch RJ, Gonzalez-Serratos H. Lateral force transmission across costameres in skeletal muscle. Exerc Sport Sci Rev. 2003 Apr;31:73-8.
Kumar A, Khandelwal N, Malya R, Reid MB, Boriek AM. Loss of dystrophin causes aberrant mechanotransduction in skeletal muscle fibers. Faseb J. 2004 Jan;18:102-13.
Bloch RJ, Reed P, O'Neill A, Strong J, Williams M, Porter N, et al. Costameres mediate force transduction in healthy skeletal muscle and are altered in muscular dystrophies. J Muscle Res Cell Motil. 2004;25:590-2.
Mariol MC, Segalat L. Muscular degeneration in the absence of dystrophin is a calcium-dependent process. Curr Biol. 2001 Oct 30;11:1691-4.
Harper SQ, Hauser MA, DelloRusso C, Duan D, Crawford RW, Phelps SF, et al. Modular flexibility of dystrophin: implications for gene therapy of Duchenne muscular dystrophy. Nature Med. 2002;8:253-61.
England S, Nicholson L, Johnson M, Forrest S, Love D, Zubrzycka-Gaarn E, et al. Very mild muscular dystrophy associated with the deletion of 46% of the dystrophin. Nature. 1990;343:180-2.
Seto JT, Ramos JN, Muir L, Chamberlain JS, Odom GL. Gene replacement therapies for duchenne muscular dystrophy using adeno-associated viral vectors. Curr Gene Ther. 2012 Jun;12:139-51.
Fairclough RJ, Wood MJ, Davies KE. Therapy for Duchenne muscular dystrophy: renewed optimism from genetic approaches. Nat Rev Genet. 2013 Jun;14:373-8.
Jarmin S, Kymalainen H, Popplewell L, Dickson G. New developments in the use of gene therapy to treat Duchenne muscular dystrophy. Expert Opin Biol Ther. 2014 Feb;14:209-30.
McGreevy JW, Hakim CH, McIntosh MA, Duan D. Animal models of Duchenne muscular dystrophy: from basic mechanisms to gene therapy. Dis Model Mech. 2015 Mar;8:195-213.
Gregorevic P, Blankinship MJ, Allen JM, Chamberlain JS. Systemic microdystrophin gene delivery improves skeletal muscle structure and function in old dystrophic mdx mice. Mol Ther. 2008 Apr;16:657-64.
Foster H, Sharp PS, Athanasopoulos T, Trollet C, Graham IR, Foster K, et al. Codon and mRNA sequence optimization of microdystrophin transgenes improves expression and physiological outcome in dystrophic mdx mice following AAV2/8 gene transfer. Mol Ther. 2008 Nov;16:1825-32.
Goyenvalle A, Vulin A, Fougerousse F, Leturcq F, Kaplan J, Garcia L, et al. Rescue of dystrophic muscle through U7 snRNA-mediated exon skipping. Science. 2004;306.
Aartsma-Rus A, Janson AA, Heemskerk JA, De Winter CL, Van Ommen GJ, Van Deutekom JC. Therapeutic modulation of DMD splicing by blocking exonic splicing enhancer sites with antisense oligonucleotides. Ann N Y Acad Sci. 2006 Oct;1082:74-6.
Aartsma-Rus A, Janson AA, Kaman WE, Bremmer-Bout M, van Ommen GJ, den Dunnen JT, et al. Antisense-induced multiexon skipping for Duchenne muscular dystrophy makes more sense. Am J Hum Genet. 2004 Jan;74:83-92.
Takeshima Y, Yagi M, Wada H, Ishibashi K, Nishiyama A, Kakumoto M, et al. Intravenous infusion of an antisense oligonucleotide results in exon skipping in muscle dystrophin mRNA of Duchenne muscular dystrophy. Pediatr Res. 2006 May;59:690-4.
McClorey G, Moulton HM, Iversen PL, Fletcher S, Wilton SD. Antisense oligonucleotide-induced exon skipping restores dystrophin expression in vitro in a canine model of DMD. Gene Ther. 2006 Oct;13:1373-81.
Vulin A, Barthelemy I, Goyenvalle A, Thibaud JL, Beley C, Griffith G, et al. Muscle function recovery in golden retriever muscular dystrophy after AAV1-U7 exon skipping. Mol Ther. 2012 Nov;20:2120-33.
Aartsma-Rus A, Muntoni F. 194th ENMC international workshop. 3rd ENMC workshop on exon skipping: towards clinical application of antisense-mediated exon skipping for Duchenne muscular dystrophy 8-10 December 2012, Naarden, The Netherlands. Neuromuscul Disord. 2013 Nov;23:934-44.
Le Guiner C, Montus M, Servais L, Cherel Y, Francois V, Thibaud JL, et al. Forelimb treatment in a large cohort of dystrophic dogs supports delivery of a recombinant AAV for exon skipping in Duchenne patients. Mol Ther. 2014 Nov;22:1923-35.
van Deutekom JC, Janson AA, Ginjaar IB, Frankhuizen WS, Aartsma-Rus A, Bremmer-Bout M, et al. Local dystrophin restoration with antisense oligonucleotide PRO051. N Engl J Med. 2007 Dec 27;357:2677-86.
Kinali M, Arechavala-Gomeza V, Feng L, Cirak S, Hunt D, Adkin C, et al. Local restoration of dystrophin expression with the morpholino oligomer AVI-4658 in Duchenne muscular dystrophy: a single-blind, placebo-controlled, dose-escalation, proof-of-concept study. Lancet Neurol. 2009 Oct;8:918-28.
Goemans NM, Tulinius M, van den Akker JT, Burm BE, Ekhart PF, Heuvelmans N, et al. Systemic administration of PRO051 in Duchenne's muscular dystrophy. N Engl J Med. 2011 Apr 21;364:1513-22.
Cirak S, Arechavala-Gomeza V, Guglieri M, Feng L, Torelli S, Anthony K, et al. Exon skipping and dystrophin restoration in patients with Duchenne muscular dystrophy after systemic phosphorodiamidate morpholino oligomer treatment: an open-label, phase 2, dose-escalation study. Lancet. 2011 Aug 13;378:595-605.
Cirak S, Feng L, Anthony K, Arechavala-Gomeza V, Torelli S, Sewry C, et al. Restoration of the Dystrophin-associated Glycoprotein Complex After Exon Skipping Therapy in Duchenne Muscular Dystrophy. Mol Ther. 2011 Nov 15.
Guiraud S, Aartsma-Rus A, Vieira NM, Davies KE, van Ommen GJ, Kunkel LM. The Pathogenesis and Therapy of Muscular Dystrophies. Annu Rev Genomics Hum Genet. 2015 Jun 4.
Wilton SD, Veedu RN, Fletcher S. The emperor's new dystrophin: finding sense in the noise. Trends Mol Med. 2015 May 23.
Findlay AR, Wein N, Kaminoh Y, Taylor LE, Dunn DM, Mendell JR, et al. Clinical phenotypes as predictors of the outcome of skipping around DMD exon 45. Ann Neurol. 2015 Jan 21;77:668-74.
Nicolas A, Raguenes-Nicol C, Ben Yaou R, Ameziane-Le Hir S, Cheron A, Vie V, et al. Becker muscular dystrophy severity is linked to the structure of dystrophin. Hum Mol Genet. 2015 Oct 27;24:1267-79.
Cacchiarelli D, Martone J, Girardi E, Cesana M, Incitti T, Morlando M, et al. MicroRNAs involved in molecular circuitries relevant for the Duchenne muscular dystrophy pathogenesis are controlled by the dystrophin/nNOS pathway. Cell Metab. 2010 Oct 6;12:341-51.
Cacchiarelli D, Incitti T, Martone J, Cesana M, Cazzella V, Santini T, et al. miR-31 modulates dystrophin expression: new implications for Duchenne muscular dystrophy therapy. EMBO Rep. 2011 Feb;12:136-41.
Kerst B, Mennerich D, Schuelke M, Stoltenburg-Didinger G, von Moers A, Gossrau R, et al. Heterozygous myogenic factor 6 mutation associated with myopathy and severe course of Becker muscular dystrophy. Neuromuscul Disord. 2000;10:572-7.
Davis DB, Delmonte AJ, Ly CT, McNally EM. Myoferlin, a candidate gene and potential modifier of muscular dystrophy. Hum Mol Genet. 2000 Jan 22;9:217-26.
Pegoraro E, Hoffman EP, Piva L, Gavassini BF, Cagnin S, Ermani M, et al. SPP1 genotype is a determinant of disease severity in Duchenne muscular dystrophy. Neurology. 2011 Jan 18;76:219-26.
Bello L, Piva L, Barp A, Taglia A, Picillo E, Vasco G, et al. Importance of SPP1 genotype as a covariate in clinical trials in Duchenne muscular dystrophy. Neurology. 2012 Jul 10;79:159-62.
Flanigan KM, Ceco E, Lamar KM, Kaminoh Y, Dunn DM, Mendell JR, et al. LTBP4 genotype predicts age of ambulatory loss in Duchenne muscular dystrophy. Ann Neurol. 2013 Apr;73:481-8.
Downloads
Additional Files
Published
How to Cite
Accepted 2015-07-20
Published 2015-07-20