The association between brain natriuretic peptide and tissue Doppler parameters in children with hypertrophic cardiomyopathy
DOI:
https://doi.org/10.17305/bjbms.2016.670Keywords:
Hypertrophic cardiomyopathy, molecular genetics, brain natriuretic peptide, tissue Doppler flow, left ventricular outflow tract obstructionAbstract
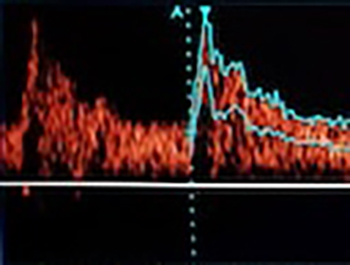
In this study, we investigated the association between brain natriuretic peptide (BNP) levels and tissue Doppler imaging measurements and also screening for deadly mutations in patients with hypertrophic cardiomyopathy (HCM). We enrolled 20 patients diagnosed with HCM (age:10.7±5 years (1-17), 85% male, weight:42.25±23.10 kg, height:141.80±32.45 cm) and 20 age, gender and body weight-matched control subjects. We performed electrocardiography, transthoracic echocardiography, and tissue Doppler echocardiography in each group, as well as genetic tests (for Arg403Gln, Arg453Cys, Arg719Trp and Arg719Gln mutations in MYH7 Exons 13, 14, 19) and BNP in the patients. The patients were divided into two groups according to the presence (Group 1) or absence (Group 2) of left ventricular (LV) outflow tract obstruction. QTc dispersion and the LV ejection fraction and left atrial (LA) volume index were increased in Group 1. The LA volume index and the mitral and septal E/Ea ratio and septum Z-score were increased while the mitral lateral annulus and septal annulus Ea wave velocities and the mitral and tricuspid E/A ratio were decreased in patients with high levels of BNP compared to those with normal BNP levels. There were no mutations that are associated with increased risk of sudden death found in patients included in this study. In the light of our data, we conclude that such parameters BNP levels above the 98 pg/mL, septal thickness Z-score ˃6, and higher mitral and septal E/Ea ratios can be used for management of patients with HCM according to life-threatening conditions.
Citations
Downloads
References
Marian AJ, Roberts R. Recent advances in the molecular genetics of hypertrophic cardiomyopathy. Circulation 1995;92(5):1336-47. http://dx.doi.org/10.1161/01.CIR.92.5.1336.
Maron BJ, Maron MS. Hypertrophic cardiomyopathy. Lancet 2013;381(9862):242-55. http://dx.doi.org/10.1016/S0140-6736(12)60397-3.
Nagueh SF, McFalls J, Meyer D, Hill R, Zoghbi WA, Tam JW, et al. Tissue doppler imaging predicts the development of hypertrophic cardiomyopathy in subjects with subclinical disease. Circulation 2003;108(4):395-8. http://dx.doi.org/10.1161/01.CIR.0000084500.72232.8D.
Dokainish H, Zoghbi WA, Lakkis NM, Al-Bakshy F, Dhir M, Quinones MA, et al. Optimal noninvasive assessment of left ventricular filling pressures: A comparison of tissue Doppler echocardiography and B-type natriuretic peptide in patients with pulmonary artery catheters. Circulation 2004;109(20):2432-9. http://dx.doi.org/10.1161/01.CIR.0000084500.72232.8D.
Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quiñones MA. Doppler tissue imaging: A noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 1997;30(6):1527-33. http://dx.doi.org/10.1016/S0735-1097(97)00344-6.
Nagueh SF, Rao L, Soto J, Middleton KJ, Khoury DS. Haemodynamic insights into the effects of ischaemia and cycle length on tissue Doppler-derived mitral annulus diastolic velocities. Clin Sci (Lond) 2004;106(2):147-54. http://dx.doi.org/10.1042/CS20030204.
Maron BJ, Epstein SE. Hypertrophic cardiomyopathy. Recent observations regarding the specificity of three hallmarks of the disease: asymmetric septal hypertrophy, septal disorganization and systolic anterior motion of the anterior mitral leaflet. Am J Cardiol 1980;45:141-54. http://dx.doi.org/10.1016/0002-9149(80)90232-5.
Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, et al. 2011 ACCF/AHA Guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: Executive summary: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011;124:2761-96. http://dx.doi.org/10.1161/CIR.0b013e318223e230.
Jaenicke T, Diederich KW, Haas W, Schleich J, Lichter P, Pfordt M, et al. The complete sequence of the human beta-myosin heavy chain gene and a comparative analysis of its product. Genomics 1990;8(2):194-206. http://dx.doi.org/10.1016/0888-7543(90)90272-V.
Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: Results of a survey of echocardiographic measurements. Circulation 1978;58(6):1072-83. http://dx.doi.org/10.1161/01.CIR.58.6.1072.
Yu CM, Sanderson JE, Marwick TH, Oh JK. Tissue Doppler imaging a new prognosticator for cardiovascular diseases. J Am Coll Cardiol 2007;49(19):1903-14. http://dx.doi.org/10.1016/j.jacc.2007.01.078.
Harada K, Tamura M, Yasuoka K, Toyono M. A comparison of tissue Doppler imaging and velocities of transmitral flow in children with elevated left ventricular preload. Cardiol Young 2001;11(3):261-8. http://dx.doi.org/10.1017/S1047951101000270.
Moe GW, Angus C, Howard RJ, De Bold AJ, Armstrong PW. Pathophysiological role of changing atrial size and pressure in modulation of atrial natriuretic factor during evolving experimental heart failure. Cardiovasc Res 1990;24(7):570-7. http://dx.doi.org/10.1093/cvr/24.7.570.
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, et al. Echocardiographic assessment of left ventricular hypertrophy: Comparison to necropsy findings. Am J Cardiol 1986;57(6):450-8. http://dx.doi.org/10.1016/0002-9149(86)90771-X.
Tei C, Ling LH, Hodge DO, Bailey KR, Oh JK, Rodeheffer RJ, et al. New index of combined systolic and diastolic myocardial performance: A simple and reproducible measure of cardiac function – A study in normals and dilated cardiomyopathy. J Cardiol 1995;26(6):357-66.
Geske JB, McKie PM, Ommen SR, Sorajja P. B-type natriuretic peptide and survival in hypertrophic cardiomyopathy. J Am Coll Cardiol 2013;61(24):2456-60. http://dx.doi.org/10.1016/j.jacc.2013.04.004.
McKenna W, Deanfield J, Faruqui A, England D, Oakley C, Goodwin J. Prognosis in hypertrophic cardiomyopathy: Role of age and clinical, electrocardiographic and hemodynamic features. Am J Cardiol 1981;47(3):532-8. http://dx.doi.org/10.1016/0002-9149(81)90535-X.
Maron BJ, Roberts WC, Epstein SE. Sudden death in hypertrophic cardiomyopathy: A profile of 78 patients. Circulation 1982;65(7):1388-94. http://dx.doi.org/10.1161/01.CIR.65.7.1388.
Chiu C, Bagnall RD, Ingles J, Yeates L, Kennerson M, Donald JA, et al. Mutations in alpha-actinin-2 cause hypertrophic cardiomyopathy: A genome-wide analysis. J Am Coll Cardiol 2010;55(11):1127-35. http://dx.doi.org/10.1016/j.jacc.2009.11.016.
Wang J, Xu SJ, Zhou H, Wang LJ, Hu B, Fang F, et al. A novel mutation of the beta myosin heavy chain gene responsible for familial hypertrophic cardiomyopathy. Clin Cardiol 2009;32(9):E16-21. http://dx.doi.org/10.1002/clc.20520.
Hirota T, Kubo T, Kitaoka H, Hamada T, Baba Y, Hayato K, et al. A novel cardiac myosin-binding protein C S297X mutation in hypertrophic cardiomyopathy. J Cardiol 2010;56(1):59-65. http://dx.doi.org/10.1016/j.jjcc.2010.02.004.
Butera G, Bonnet D, Kachaner J, Sidi D, Villain E. Heart rate variability in children with hypertrophic cardiomyopathy. Heart 2003;89(2):205-6. http://dx.doi.org/10.1136/heart.89.2.205.
Yi G, Poloniecki J, Dickie S, Elliott PM, Malik M, McKenna WJ. Is QT dispersion associated with sudden cardiac death in patients with hypertrophic cardiomyopathy? Ann Noninvasive Electrocardiol 2001;6(3):209-15. http://dx.doi.org/10.1111/j.1542-474X.2001.tb00110.x.
Miorelli M, Buja G, Melacini P, Fasoli G, Nava A. QT-interval variability in hypertrophic cardiomyopathy patients with cardiac arrest. Int J Cardiol 1994;45(2):121-7. http://dx.doi.org/10.1016/0167-5273(94)90267-4.
Göktekin O, Ritsushi K, Matsumoto K, Hiroshi M. The relationship between QT dispersion and risk factors of sudden death in hypertrophic cardiomyopathy. Anadolu Kardiyol Derg 2002;2(3):226-30.
Brito D, Matias JS, Sargento L, Cabral MJ, Madeira HC. Plasma N-terminal pro-brain natriuretic peptide: A marker of left ventricular hypertrophy in hypertrophic cardiomyopathy. Rev Port Cardiol 2004;23(12):1557-82.
Nishigaki K, Tomita M, Kagawa K, Noda T, Minatoguchi S, Oda H, et al. Marked expression of plasma brain natriuretic peptide is a special feature of hypertrophic obstructive cardiomyopathy. J Am Coll Cardiol 1996;28(5):1234-42. http://dx.doi.org/10.1016/S0735-1097(96)00277-X.
Kaski JP, Tomé-Esteban MT, Mead-Regan S, Pantazis A, Marek J, Deanfield JE, et al. B-type natriuretic peptide predicts disease severity in children with hypertrophic cardiomyopathy. Heart 2008;94(10):1307-11. http://dx.doi.org/10.1136/hrt.2007.126748.
El-Saiedi SA, Seliem ZS, Esmail RI. Hypertrophic cardiomyopathy: Prognostic factors and survival analysis in 128 Egyptian patients. Cardiol Young 2014;24(4):702-8. http://dx.doi.org/10.1017/S1047951113001030.
Decker JA, Rossano JW, Smith EO, Cannon B, Clunie SK, Gates C, et al. Risk factors and mode of death in isolated hypertrophic cardiomyopathy in children. J Am Coll Cardiol 2009;54(3):250-4. http://dx.doi.org/10.1016/j.jacc.2009.03.051.
Nagueh SF, Bachinski LL, Meyer D, Hill R, Zoghbi WA, Tam JW, et al. Tissue Doppler imaging consistently detects myocardial abnormalities in patients with hypertrophic cardiomyopathy and provides a novel means for an early diagnosis before and independently of hypertrophy. Circulation 2001;104(2):128-30. http://dx.doi.org/10.1161/01.CIR.104.2.128.
McMahon CJ, Nagueh SF, Pignatelli RH, Denfield SW, Dreyer WJ, Price JF, et al. Characterization of left ventricular diastolic function by tissue Doppler imaging and clinical status in children with hypertrophic cardiomyopathy. Circulation 2004;109(14):1756-62. http://dx.doi.org/10.1161/01.CIR.0000124723.16433.31.
Matsumura Y, Elliott PM, Virdee MS, Sorajja P, Doi Y, McKenna WJ. Left ventricular diastolic function assessed using Doppler tissue imaging in patients with hypertrophic cardiomyopathy: Relation to symptoms and exercise capacity. Heart 2002;87(3):247-51. http://dx.doi.org/10.1136/heart.87.3.247.
Kitaoka H, Kubo T, Hayashi K, Yamasaki N, Matsumura Y, Furuno T, et al. Tissue doppler imaging and prognosis in asymptomatic or mildly symptomatic patients with hypertrophic cardiomyopathy. Eur Heart J Cardiovasc Imaging 2013;14(6):544-9. http://dx.doi.org/10.1093/ehjci/jes200.
Kitaoka H, Kubo T, Okawa M, Takenaka N, Sakamoto C, Baba Y, et al. Tissue Doppler imaging and plasma BNP levels to assess the prognosis in patients with hypertrophic cardiomyopathy. J Am Soc Echocardiogr 2011;24(9):1020-5. http://dx.doi.org/10.1016/j.echo.2011.05.009.
Downloads
Additional Files
Published
Issue
Section
Categories
How to Cite
Accepted 2015-09-21
Published 2016-01-01









